Influence of LMR and LMR/LDH on Prognosis of Primary Waldeyer's Ring Diffuse Large B-cell Lymphoma
-
摘要:目的
探讨外周血LMR和LMR/LDH在原发韦氏环弥漫性大B细胞淋巴瘤(DLBCL)患者预后中的预测价值。
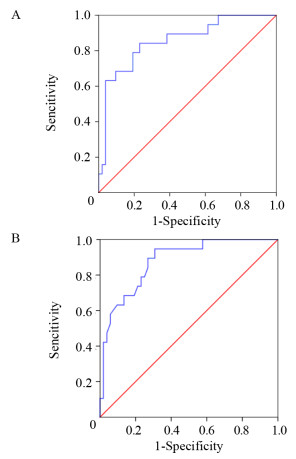
方法收集71例原发韦氏环DLBCL患者临床资料,采用ROC曲线确定患者治疗前外周血LMR、LMR/LDH的最佳临界值,卡方检验分析LMR高低组和LMR/LDH高低组构成比和率。生存率的比较采用Kaplan-Meier法,单因素分析用Log rank法检验,多因素分析用Cox风险回归模型。
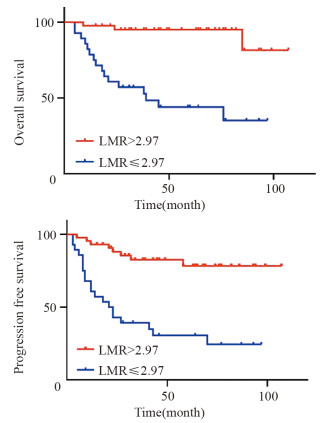
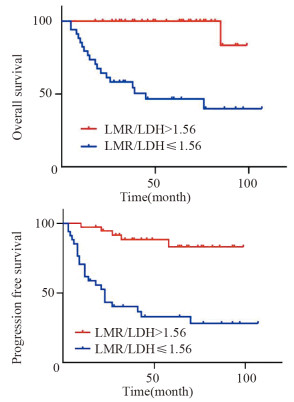
结果LMR和LMR/LDH临界值分别为2.97和1.56。高LMR组患者的预后明显优于低LMR组(P < 0.001);高LMR/LDH组患者的预后明显优于低LMR/LDH组(P < 0.001)。单因素分析显示年龄、B症状、临床分期、治疗疗效、IPI评分、LDH水平、LMR及LMR/LDH是影响早期韦氏环DLBCL患者预后的重要因素;多因素分析显示LMR/LDH、年龄、临床分期是其独立预后因素。
结论治疗前LMR和LMR/LDH在韦氏环DLBCL患者预后中可能具有一定的预测价值。
-
关键词:
- 弥漫性大B细胞淋巴瘤 /
- 韦氏环 /
- 淋巴细胞/单核细胞 /
- 乳酸脱氢酶 /
- 预后
Abstract:ObjectiveTo investigate the predictive value of peripheral blood LMR and LMR/LDH on the prognosis of primary Waldeyer's Ring DLBCL patients.
MethodsWe collected 71 patients with primary Waldeyer's Ring DLBCL. The ROC curve was used to determine the optimal critical values of LMR and LMR/LDH before treatment. The chi-square test was used to analyze the constituent ratio and rate of high and low LMR groups as well as high and low LMR/LDH groups. Kaplan-Meier method was used to calculate survival rate. Log rank method and Cox risk regression model were used for univariate and multivariate analyses, respectively.
ResultsThe optimal critical values of LMR and LMR/LDH were 2.97 and 1.56, respectively. The prognosis of patients in the high LMR group was significantly better than that in the low LMR group (P < 0.001). The prognosis of patients in the high LMR/LDH group was significantly better than that in the low LMR/LDH group (P < 0.001). Univariate analysis showed that age, B symptoms, clinical stage, treatment efficacy, IPI score, LDH level, LMR and LMR/LDH were important factors that influenced the prognosis of early-stage Waldeyer's Ring DLBCL. Multivariate analysis showed that the age, clinical stage and LMR/LDH were independent prognostic factors.
ConclusionLMR and LMR/LDH before treatment may have certain value in predicting the prognosis of Waldeyer's Ring DLBCL patients.
-
0 引言
韦氏环是指包含扁桃体、口咽、鼻咽、舌根以及软腭在内的环状淋巴组织。国外报道原发韦氏环淋巴瘤占全部非霍奇金淋巴瘤(non-Hodgkin's lymphoma, NHL)患者的5%~10%[1],我国及亚洲地区多见,约占同期全部NHL患者的10%~20%[2-3],是最常见的头颈部NHL。NHL的所有病理亚型均可出现在韦氏环部位,以侵袭性淋巴瘤为主,弥漫性大B细胞淋巴瘤(diffuse large B-cell lymphoma,DLBCL)占韦氏环NHL的50%~80%[4-6]。
DLBCL是一类在免疫表型、致病因素和临床反应及预后因素等多方面具有高度异质性的全身性恶性疾病,但具有潜在可治愈性。因此,需要有效的临床预后生物标志物来预测预后。国际预后指数(international prognostic index,IPI)是目前临床恶性淋巴瘤预后危险分层的基础,广泛应用于临床预后评估。研究显示[7-8],DLBCL传统化疗方案加入利妥昔单抗后,各危险组的生存显著改善,IPI评分预后价值下降,因此应确定新的、简单、快速、重复性高且有效的生物标志物,对患者进行预后危险分层,提供个体化治疗。免疫缺陷是NHL最广泛描述的危险因素之一[9],先天性或获得性全身免疫抑制的患者淋巴瘤患病风险更高[10-11]。基因表达谱(GEP)研究表明DLBCL生存结局不仅由临床参数决定,还由与调节肿瘤微环境相关的基因决定[12],但寻找基于基因水平的预后指标价格昂贵且不易获得,无法广泛应用。近年来,基于免疫及肿瘤微环境的预后因素如外周血淋巴细胞与单核细胞比值(lymphocyte to monocyte ratio, LMR)、LMR与乳酸脱氢酶比值(LMR to lactate dehydrogenase level ratio, LMR/LDH)先后被探索,它们被认为是包括DLBCL[13-15]在内的多种恶性肿瘤的重要预后指标。本研究旨在探索LMR以及LMR/LDH在原发韦氏环DLBCL患者预后中的预测价值。
1 资料与方法
1.1 研究对象
收集2011年10月—2019年10月宁夏医科大学总医院收治的具有完整临床资料,且经病理活检及免疫组织化学检测明确诊断的韦氏环DLBCL患者71例。纳入标准:淋巴瘤原发于韦氏环、免疫组织化学检测为CD20阳性、初始治疗于我院、一线化疗方案为CHOP±R方案(环磷酰胺+多柔比星/表柔比星+长春新碱+泼尼松±利妥昔单抗)、有完整的随访资料者。排除标准:淋巴瘤继发于韦氏环、患有其他恶性肿瘤病史或严重危及生命的疾病以及随访资料不完整者。
1.2 研究指标
从患者初始治疗前一周内检测的外周血实验室指标中获得绝对淋巴细胞计数(absolute lymphocyte count, ALC)、绝对单核细胞计数(absolute monocyte count, AMC)及血清乳酸脱氢酶(lactate dehydrogenase, LDH),LMR为ALC与AMC的比值,LMR/LDH为LMR与LDH的比值。收集患者治疗前年龄、B症状、ECOG评分、LDH水平、IPI评分、Ann Arbor分期、Hans分型、原发部位、治疗疗效、LMR、LMR/LDH等临床资料。
1.3 观察终点
总生存时间(overall survival, OS)是指从确诊日期开始至由任何原因导致受试者死亡的日期或随访截止日期(2020年10月)的时间。无疾病进展生存期(progression free survival, PFS)是指从确诊日期开始至肿瘤复发、转移或由任何原因导致受试者死亡的时间。失访、死于其他疾病或突发事件和随访截止时仍未发生死亡的情况均定为删失数据。
1.4 统计学方法
采用SPSS23.0软件进行统计分析,ROC曲线确定LMR、LMR/LDH的最佳临界值,卡方检验分析LMR高、低组及LMR/LDH高、低组构成比和率。使用Kaplan-Meier法绘制生存曲线,Log rank检验比较生存率。采用Kaplan-Meier法进行单因素分析,Cox风险回归模型进行多因素分析,P < 0.05为差异有统计学意义。
2 结果
2.1 随访结果
共纳入原发韦氏环DLBCL患者71例,其中男性41例(58%),女性30例(42%),男女比例为1.37:1,其中大于60岁者27例(38%),中位发病年龄56岁。根据Ann Arbor分期Ⅰ~Ⅱ期50例(70%),Ⅲ~Ⅳ期21例(30%)。全组5年OS和PFS分别为74.2%和58.7%。全组中位随访时间45月(5~107月),所有患者均通过门诊复诊记录及电话联系完成随访,随访率100%。共19例患者死亡,其中14例因原发肿瘤死亡,4例死于治疗相关并发症,1例死于其他肿瘤疾病。
2.2 LMR和LMR/LDH临界值的确定
根据生存情况,使用ROC曲线计算治疗前LMR、LMR/LDH的曲线下面积(AUC)分别为0.855(95%CI: 0.753~0.958)、0.878(95%CI: 0.794~0.962)。根据ROC曲线确定临界值:LMR为2.97,LMR/LDH为1.56。根据临界值进行分组,大于临界值为高组,小于等于临界值为低组。ROC曲线见图 1。
2.3 LMR、LMR/LDH与患者临床特征的相关性
结果显示,与LMR > 2.97组比较,LMR≤2.97更倾向于发生在高龄、Ann Arbor分期较晚、IPI评分较高、LDH高于正常上限(250 u/L)的原发韦氏环DLBCL患者中,LMR/LDH≤1.56与LMR有相同趋势,见表 1。
表 1 原发韦氏环DLBCL患者临床特征与LMR、LMR/LDH之间的相关性(n=71)Table 1 Relation between clinical features and LMR, LMR/LDH in primary Waldeyer's Ring DLBCL patients (n=71)
2.4 LMR、LMR/LDH与患者预后的关系
Kaplan-Meier生存曲线结果显示,LMR > 2.97组的预后明显优于LMR≤2.97组,5年OS、PFS分别为95.1% vs. 44.0%(P < 0.001)、78.2% vs. 30.6%(P < 0.001),见图 2。LMR/LDH > 1.56组的预后明显优于LMR/LDH≤1.56组,5年OS、PFS分别为100.0% vs. 44.6%(P < 0.001)、83.1% vs. 32.9%(P < 0.001),见图 3。
2.5 影响原发韦氏环DLBCL患者预后因素分析
2.5.1 单因素分析
结果显示:年龄、Ann Arbor分期、IPI评分、LDH水平、治疗疗效、LMR和LMR/LDH为影响韦氏环DLBCL患者预后的危险因素,见表 2。
表 2 影响原发韦氏环DLBCL患者预后的单因素分析(n=71)Table 2 Univariate analysis of prognostic factors in patients with primary Waldeyer's Ring DLBCL (n=71)
2.5.2 多因素分析
结果显示,LMR/LDH比值为OS和PFS的独立预后标志物。此外,OS与年龄显著相关,PFS与年龄和Ann Arbor分期显著相关,是DLBCL的独立预后不良因素,见表 3。
表 3 影响原发韦氏环DLBCL患者预后的多因素分析(n=71)Table 3 Multivariate analysis of prognostic factors in patients with primary Waldeyer's Ring DLBCL (n=71)
3 讨论
在一些实体肿瘤中,全血细胞计数(CBC)参数的预后意义已经被证实[16]。其中单核细胞计数与机体炎性反应相关,淋巴细胞计数与机体免疫状态有关[17-18]。淋巴细胞是机体重要的免疫效应细胞,在正常机体内起免疫监视的作用,其减少是宿主免疫缺陷的重要标志[19],常预示侵袭性恶性淋巴瘤的不良预后[20]。单核细胞作用与之相反,可抑制体内抗肿瘤免疫反应,也可通过浸润肿瘤部位并分化为肿瘤相关巨噬细胞,后者通过分泌具有抗肿瘤活性及促血管生成和免疫抑制的细胞因子及趋化因子,在肿瘤进展、转移、血管生成和免疫耐受中起重要作用,从而影响DLBCL的预后[19, 21-22]。因此,绝对淋巴细胞计数(absolute lymphocyte count, ALC)的减低和绝对单核细胞计数(absolute monocyte count, AMC)的增高都是DLBCL患者的不良预后因素。在肿瘤微环境中,炎性反应、免疫状态都发挥着重要作用,ALC与AMC比值即LMR将宿主免疫和肿瘤微环境作为一个生物系统联合评价,更能准确反映宿主的免疫状态。Bento等[23]单因素分析结果显示CBC参数中ALC、AMC、LMR、红细胞分布宽度等都对DLBCL患者有显著预后价值,但多因素分析只有LMR及RDW是OS和PFS的独立预后因素。蔡春颖等[24]研究显示,LMR和IPI是影响淋巴瘤OS的两个独立预后因素,但对淋巴瘤DFS有影响的因素是LMR而非IPI。Zhou等[25]研究也表明诊断和完成一线化疗时维持高LMR是DLBCL患者PFS和OS的独立预后因素。低LMR组以及治疗完成后LMR未能从诊断时的低水平恢复的患者预后较差。近期文献显示,患者的生存不仅受宿主体内免疫反应的影响,还受肿瘤固有特征的影响,如肿瘤的基因突变、病理类型和肿瘤大小等[26-27],最重要的是淋巴细胞或单核细胞的水平和功能可能由肿瘤细胞调节[28]。因此单用LMR可能不是预测患者临床生存的完美预测指标,结合肿瘤负荷更能有效预测DLBCL患者的预后。Nguyen等[29]研究显示FDG-PET/CT参数值中的最大标准摄取值(SUVmax)可反映DLBCL患者肿瘤负荷,但由于其价格昂贵,不能医保报销,使用常常受限。相关报道LDH升高与细胞增殖相关,被认为是高肿瘤负荷的标志,是肿瘤预后不良的因素[30-31]。LDH水平升高是肿瘤糖酵解活性增强和缺氧导致肿瘤坏死的产物,而肿瘤坏死在存在大肿块的肿瘤患者中发生率更高,这解释了高肿瘤负荷患者的高LDH水平。综上,LDH可能在一定程度上能反映DLBCL患者的肿瘤负荷。为评估血清LDH水平是否能够反映DLBCL患者的肿瘤负荷,Ji等[15]采用Spearman相关分析方法,测定了血清LDH水平与PET-CT检测肿瘤水平呈显著正相关(P < 0.01),相关系数为0.78。杨迪等[32]的研究也得出相似结果。综上,LDH可能在一定程度上能反映DLBCL患者的肿瘤负荷。此外,LDH与肿瘤的免疫反应之间也存在密切联系,在肿瘤微环境中,肿瘤细胞的增殖需要大量的葡萄糖提供能量,而葡萄糖缺乏以及肿瘤细胞的高糖酵解速率产生的大量乳酸会削弱肿瘤微环境中免疫细胞的功能,从而产生抑制效应[33]。此外高乳酸会促进肿瘤相关巨噬细胞(TAMs)极化为M2巨噬细胞,从而导致免疫抑制[34]。因此,结合肿瘤免疫与肿瘤负荷的预后指标LMR/LDH可能更能有效预测DLBCL患者的预后。
本研究显示,LMR/LDH是OS和PFS独立预后因素,而IPI评分、LMR和LDH,无论是OS(P=0.930, P=0.935, P=0.875)还是PFS(P=0.861, P=0.684, P=0.854)结果均不显著,本研究结果与Ji等[15]及杨迪[32]等研究结果一致。采用LMR/LDH单一因素预测预后结果存在偏倚,因本研究为回顾性、单中心、小样本研究,结果支持LMR、LMR/LDH在原发韦氏环DLBCL患者预后中存在一定的价值,但未能将其联合其他预后因素形成新的预后评分系统对患者进行危险分层,进一步探讨其预后能力。
综上所述,为了实现DLBCL患者的个体化治疗,同时避免治疗不足和过度治疗,从而提高治愈率,简单、快速、有效的预后标志物具有重要意义。目前研究大多支持LMR、LMR/LDH等结合肿瘤免疫相关的指标在DLBCL患者预后中存在一定的价值。这些指标可以在临床预后评分系统的基础上对DLBCL患者进行进一步预后分层[23, 35],但并没有被普遍采用,部分原因可能是因为LMR及LMR/LDH最佳临界值的确定受诸多因素,如年龄、免疫功能状态、感染或其他炎性反应疾病及样本量等影响。目前研究大多为回顾性且样本量有限,各研究结果LMR、LMR/LDH临界值不一,尚需要前瞻性、大样本、多中心研究确定并对其预后价值进一步研究。
Competing interests: The authors declare that they have no competing interests.作者贡献:刘琦:收集数据、撰写论文郭鹏:收集数据詹文华:指导论文写作、修改论文 -
表 1 原发韦氏环DLBCL患者临床特征与LMR、LMR/LDH之间的相关性(n=71)
Table 1 Relation between clinical features and LMR, LMR/LDH in primary Waldeyer's Ring DLBCL patients (n=71)

表 2 影响原发韦氏环DLBCL患者预后的单因素分析(n=71)
Table 2 Univariate analysis of prognostic factors in patients with primary Waldeyer's Ring DLBCL (n=71)

表 3 影响原发韦氏环DLBCL患者预后的多因素分析(n=71)
Table 3 Multivariate analysis of prognostic factors in patients with primary Waldeyer's Ring DLBCL (n=71)

-
[1] Krol ADG, Le Cessie S, Snijder S, et al. Primary extranodal non-Hodgkin's lymphoma (NHL): the impact of alternative definitions tested in the Comprehensive Cancer Centre West population-based NHL registry[J]. Ann Oncol, 2003, 14(1): 131-139. doi: 10.1093/annonc/mdg004
[2] Wu RY, Li YX, Wang WH, et al. Clinical disparity and favorable prognoses for patients with Waldeyer ring extranodal nasal-type NK/T-cell lymphoma and diffuse large B-cell lymphoma[J]. Am J Clin Oncol, 2014, 37(1): 41-46. doi: 10.1097/COC.0b013e318261084b
[3] Qi SN, Li YX, Wang H, et al. Diffuse large B-cell lymphoma: clinical characterization and prognosis of Waldeyer ring versus lymph node presentation[J]. Cancer, 2009, 115(21): 4980-4989. doi: 10.1002/cncr.24557
[4] Lee SJ, Suh CW, Lee SI, et al. Clinical characteristics, pathological distribution, and prognostic factors in non-Hodgkin lymphoma of Waldeyer's ring: nationwide Korean study[J]. Korean J Intern Med, 2014, 29(3): 352-360. doi: 10.3904/kjim.2014.29.3.352
[5] Ma Z, Shi Y, Pang X, et al. Clinicopathologic features and prognostic analysis of Waldeyer ring B-cell lymphoma[J]. Medicine (Baltimore), 2020, 99(2): e18670. doi: 10.1097/MD.0000000000018670
[6] 高大林, 付骞千, 张甜甜, 等. 112例原发性韦氏环淋巴瘤的临床病理特征及预后分析[J]. 中国实验血液学杂志, 2015, 23(5): 1301-1308. https://www.cnki.com.cn/Article/CJFDTOTAL-XYSY201505018.htm Gao DL, Fu QQ, Zhang TT, et al. Analysis of Clinicopathological Characteristics and Prognosis of 112 Patients with Primary Waldeyer's Ring Lymphoma[J]. Zhongguo Shi Yan Xue Ye Xue Za Zhi, 2015, 23(5): 1301-1308. https://www.cnki.com.cn/Article/CJFDTOTAL-XYSY201505018.htm
[7] Ngo L, Hee SW, Lim LC, et al. Prognostic factors in patients with diffuse large B cell lymphoma: Before and after the introduction of rituximab[J]. Leuk Lymphoma, 2008, 49(3): 462-469. doi: 10.1080/10428190701809156
[8] 宋佳琳, 魏小磊, 张元坤, 等. IPI、NCCN-IPI及年龄调整的IPI评分系统在弥漫大B细胞淋巴瘤患者中的预后价值比较[J]. 中华血液学杂志, 2018, 39(9): 739-744. Song JL, Wei XL, Zhang YK, et al. The prognostic value of the international prognostic index, the national comprehensive cancer network IPI and the age-adjusted IPI in diffuse large B cell lymphoma[J]. Zhonghua Xue Ye Xue Za Zhi, 2018, 39(9): 739-744.
[9] Bispo JAB, Pinheiro PS, Kobetz EK. Epidemiology and Etiology of Leukemia and Lymphoma[J]. Cold Spring Harb Perspect Med, 2020, 10(6): a034819. doi: 10.1101/cshperspect.a034819
[10] Yanik EL, Smith JM, Shiels MS, et al. Cancer Risk After Pediatric Solid Organ Trans-plantation[J]. Pediatrics, 2017, 139(5): e20163893. doi: 10.1542/peds.2016-3893
[11] Fallah M, Liu X, Ji J, et al. Autoimmune diseases associated with non-Hodgkin lymphoma: a nationwide cohort study[J]. Ann Oncol, 2014, 25(10): 2025-2030. doi: 10.1093/annonc/mdu365
[12] Lenz G, Wright G, Dave SS, et al. Stromal gene signatures in large-B-cell lymphomas[J]. NEngl J Med, 2008, 359(22): 2313-2323. doi: 10.1056/NEJMoa0802885
[13] Fülöp ZZ, Gurzu S, Fülöp RL, et al. Prognostic Impact of the Neutrophil-to-Lymphocyte and Lymphocyte-to-Monocyte Ratio, in Patients with Rectal Cancer: A Retrospective Study of 1052 Patients[J]. J Pers Med, 2020, 10(4): 173. doi: 10.3390/jpm10040173
[14] Katoh D, Ochi Y, Yabushita T, et al. Peripheral Blood Lymphocyte-to-Monocyte Ratio at Relapse Predicts Outcome for Patients With Relapsed or Refractory Diffuse Large B-cell Lymphoma in the Rituximab Era[J]. Clin Lymphoma Myeloma Leuk, 2017, 17(12): e91-e97. doi: 10.1016/j.clml.2017.08.096
[15] Ji H, Niu X, Yin L, et al. Ratio of Immune Response to Tumor Burden Predicts Survival Via Regulating Functions of Lymphocytes and Monocytes in Diffuse Large B-Cell Lymphoma[J]. Cell Physiol Biochem, 2018, 45(3): 951-961. doi: 10.1159/000487288
[16] Hoshimoto S, Hishinuma S, Shirakawa H, et al. Validation and clinical usefulness of pre- and postoperative systemic inflammatory parameters as prognostic markers in patients with potentially resectable pancreatic cancer[J]. Pancreatology, 2020, 20(2): 239-246. doi: 10.1016/j.pan.2019.12.004
[17] Mohsen A, Taalab M, Abousamra N, et al. Prognostic Significance of Absolute Lymphocyte Count, Absolute Monocyte Count, and Absolute Lymphocyte Count to Absolute Monocyte Count Ratio in Follicular Non-Hodgkin Lymphoma[J]. Clin Lymphoma Myeloma Leuk, 2020, 20(9): e606-e615. doi: 10.1016/j.clml.2020.03.007
[18] Yu JI, Park HC, Yoo GS, et al. Clinical importance of the absolute count of neutrophils, lymphocytes, monocytes, and platelets in newly diagnosed hepatocellular carcinoma[J]. Sci Rep, 2021, 11(1): 2614. doi: 10.1038/s41598-021-82177-5
[19] Sawa-Wejksza K, Kandefer-Szerszeń M. Tumor-Associated Macrophages as Target for Antitumor Therapy[J]. Arch Immunol Ther Exp (Warsz), 2018, 66(2): 97-111. doi: 10.1007/s00005-017-0480-8
[20] Porrata LF, Ristow KM, Habermann TM, et al. Peripheral blood absolute lymphocyte/monocyte ratio during rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone treatment cycles predicts clinical outcomes in diffuse large B-cell lymphoma[J]. Leuk Lymphoma, 2014, 55(12): 2728-2738 doi: 10.3109/10428194.2014.893313
[21] Petty AJ, Yang Y. Tumor-associated macrophages: implications in cancer immunotherapy[J]. Immunotherapy, 2017, 9(3): 289-302. doi: 10.2217/imt-2016-0135
[22] Wen S, Chen N, Hu Y, et al. Elevated peripheral absolute monocyte count related to clinicopathological features and poor prognosis in solid tumors: Systematic review, meta-analysis, and meta-regression[J]. Cancer Med, 2021, 10(5): 1690-1714. doi: 10.1002/cam4.3773
[23] Bento L, Díaz-López A, Barranco G, et al. New prognosis score including absolute lymphocyte/monocyte ratio, red blood cell distribution width and beta-2 microglobulin in patients with diffuse large B-cell lymphoma treated with R-CHOP: Spanish Lymphoma Group Experience (GELTAMO)[J]. Br J Haematol, 2020, 188(6): 888-897. doi: 10.1111/bjh.16263
[24] 蔡春颖, 孙丽霞, 吕鸿雁. 初诊时非霍奇金淋巴瘤患者外周血淋巴细胞与单核细胞比值在预后评估中的作用[J]. 临床荟萃, 2016, 31(7): 736-740. https://www.cnki.com.cn/Article/CJFDTOTAL-LCFC201607010.htm Cai CY, Sun LX, Lyu HY. Role of peripheral blood lymphocyte to monocyte ratio during preliminary diagnosis in prognosis assessment of patients with non-Hodgkin lymphoma[J]. Lin Chuang Hui Cui, 2016, 31(7): 736-740. https://www.cnki.com.cn/Article/CJFDTOTAL-LCFC201607010.htm
[25] Zhou S, Xu L, Ma Y, et al. Peripheral blood lymphocyte to monocyte ratio recovery from low levels at diagnosis after completion of first line therapy predicts good clinical outcomes in patients with diffuse large B-cell lymphoma[J]. Oncotarget, 2017, 8(12): 19556-19565. doi: 10.18632/oncotarget.14700
[26] Leivonen SK, Taskinen M, Cervera A, et al. Alternative splicing discriminates molecular subtypes and has prognostic impact in diffuse large B-cell lymphoma[J]. Blood Cancer J, 2017, 7(8): e596. doi: 10.1038/bcj.2017.71
[27] Reddy A, Zhang J, Davis NS, et al. Genetic and Functional Drivers of Diffuse Large B Cell Lymphoma[J]. Cell, 2017, 171(2): 481-494. e15. doi: 10.1016/j.cell.2017.09.027
[28] Su S, Liu Q, Chen J, et al. A positive feedback loop between mesenchymal-like cancer cells and macrophages is essential to breast cancer metastasis[J]. Cancer Cell, 2014, 25(5): 605-620. doi: 10.1016/j.ccr.2014.03.021
[29] Nguyen XC, Lee WW, Amin AM, et al. Tumor Burden Assessed by the Maximum Standardized Uptake Value and Greatest Diameter on FDG-PET Predicts Prognosis in Untreated Diffuse Large B-cell Lymphoma[J]. Nucl Med Mol Imaging, 2010, 44(1): 39-44. doi: 10.1007/s13139-009-0009-0
[30] Huang AC, Postow MA, Orlowski RJ, et al. T-cell invigoration to tumour burden ratio associated with anti-PD-1 response[J]. Nature, 2017, 545(7652): 60-65. doi: 10.1038/nature22079
[31] Salles G, de Jong D, Xie W, et al. Prognostic significance of immunohistochemical biomarkers in diffuse large B-cell lymphoma: a study from the Lunenburg Lymphoma Biomarker Consortium[J]. Blood, 2011, 117(26): 7070-7078. doi: 10.1182/blood-2011-04-345256
[32] 杨迪, 苏丽萍. 外周血淋巴细胞/单核细胞比值(LMR)及其与乳酸脱氢酶比值对弥漫大B细胞淋巴瘤患者预后的影响[J]. 中国实验血液学杂志, 2020, 28(5): 1563-1569. https://www.cnki.com.cn/Article/CJFDTOTAL-XYSY202005028.htm Yang D, Su LP. Influence of Peripheral Blood Lymphocyte/Monocyte ratio(LMR)and Its Ratio to Lactate Dehydrogenase on Prognosis of Patients with Diffuse Large B-Cell Lymphoma[J]. Zhongguo Shi Yan Xue Ye Xue Za Zhi, 2020, 28(5): 1563-1569. https://www.cnki.com.cn/Article/CJFDTOTAL-XYSY202005028.htm
[33] Van Wilpe S, Koornstra R, Den Brok M, et al. Lactate dehydrogenase: a marker of diminished antitumor immunity[J]. Oncoimmunology, 2020, 9(1): 1731942. doi: 10.1080/2162402X.2020.1731942
[34] Colegio OR, Chu NQ, Szabo AL, et al. Functional polarization of tumour-associated macrophages by tumour-derived lactic acid[J]. Nature, 2014, 513(7519): 559-563. doi: 10.1038/nature13490
[35] Sun F, Zhu J, Lu S, et al. An inflammation-based cumulative prognostic score system in patients with diffuse large B cell lymphoma in rituximab era[J]. BMC Cancer, 2018, 18(1): 5. doi: 10.1186/s12885-017-3931-z



 下载:
下载: