Correlation of Prognostic Nutritional Index with Overall Survival of Postoperative Patients with Thymoma
-
摘要:目的
探讨预后营养指数(PNI)与胸腺瘤术后患者总生存率的相关性。
方法回顾性分析173例胸腺瘤术后患者的临床病理资料。
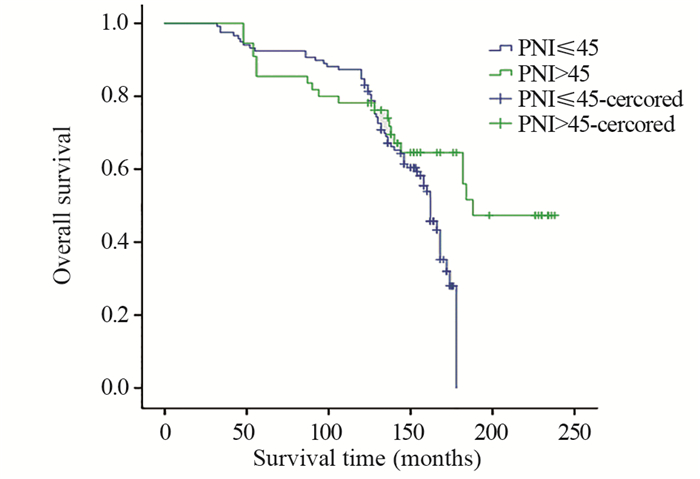
结果手术是否R0切除(P < 0.001)、是否合并重症肌无力(P < 0.001)、Masaoka分期(Ⅱ/Ⅰ: P=0.012; Ⅲ & Ⅳ/Ⅰ: P=0.011)、WHO分型(P < 0.001)和PNI(P=0.016)是影响胸腺瘤术后患者总生存率的独立危险因素。分层分析结果显示,在PNI高值组(PNI > 45)中手术是否R0切除(P=0.001)和是否合并重症肌无力(P=0.039)是影响患者总生存率的独立危险因素;在PNI低值组(PNI≤45)中Masaoka分期(Ⅱ/Ⅰ: P=0.012; Ⅲ & Ⅳ/Ⅰ: P=0.048)、WHO分型(P=0.039)、手术是否R0切除(P < 0.001)和是否合并重症肌无力(P < 0.001)是影响患者总生存率的独立危险因素。合并有重症肌无力的患者容易出现PNI降低。
结论胸腺瘤患者术后总生存率与Masaoka分期、WHO分型、手术是否完整切除、是否合并重症肌无力和预后营养指数密切相关。对于存在重症肌无力的胸腺瘤患者PNI较低,总生存率较低,应常规监测PNI。
Abstract:ObjectiveTo evaluate the correlation of prognostic nutritional index(PNI) with overall survival of postoperative patients with thymoma.
MethodsThe clinical and pathological data of 173 postoperative patients with thymoma were analyzed retrospectively.
ResultsR0 resection (P < 0.001), myasthenia gravis (P < 0.001), Masaoka stage (Ⅱ/Ⅰ: P=0.012; Ⅲ & Ⅳ/Ⅰ: P=0.011), WHO type (P < 0.001) and PNI (P=0.016) were independent risk factors for OS of postoperative patients with thymoma. R0 resection (P=0.001) and myasthenia gravis (P=0.039) were independent risk factors for OS of higher PNI group (PNI > 45); and Masaoka stage (Ⅱ/Ⅰ: P=0.012; Ⅲ & Ⅳ/Ⅰ: P=0.048), WHO type (P=0.039), R0 resection (P < 0.001) and myasthenia gravis(P < 0.001) were independent risk factors for OS of lower PNI group (PNI≤45). Patients with myasthenia gravis are prone to have a decreased PNI.
ConclusionComplete resection, myasthenia gravis, Masaoka stage, WHO type and PNI are independent prognostic factors for postoperative patients with thymoma. Thymoma patients with myasthenia gravis have lower PNI and OS. PNI should be routinely monitored in thymoma patients with myasthenia gravis.
-
Key words:
- Thymoma /
- Surgery /
- Prognostic nutritional index /
- Survival analysis
-
Competing interests: The authors declare that they have no competing interests.作者贡献:王岩:研究方向的设计论证、数据的收集和统计分析及论文的写作曹玉:数据的统计分析殷金环:数据的收集刘俊峰:论文的写作及研究的设计
-
表 1 PNI高值组和低值组胸腺瘤患者的基线特征(n(%))
Table 1 General characteristics of postoperative patients with thymoma according to PNI (n(%))

表 2 胸腺瘤术后患者总生存率影响因素的单因素分析
Table 2 Univariate analysis of influence factors for overall survival of postoperative patients with thymoma

表 3 胸腺瘤术后患者总生存率影响因素的多因素分析
Table 3 Multivariate analysis of influence factors for overall survival of postoperative patients with thymoma

表 4 胸腺瘤术后PNI≤45和PNI>45组患者总生存率影响因素的单因素分析
Table 4 Univariate analysis for influence factors for overall survival of postoperative patients with thymoma in PNI≤45 and PNI>45 groups

表 5 胸腺瘤术后PNI≤45和PNI>45患者总生存率影响因素的多因素分析
Table 5 Multivariate analysis for influence factors for OS of postoperative patients with thymoma in PNI≤45 and PNI>45 groups

-
[1] Nozoe T, Ninomiya M, Maeda T, et al. Prognostic nutritional index: a tool to predict the biological aggressiveness of gastric carcinoma[J]. Surg Today, 2010, 40(5): 440-443. doi: 10.1007/s00595-009-4065-y
[2] Kanda M, Fujii T, Kodera Y, et al. Nutritional predictors of postoperative outcome in pancreatic cancer[J]. Br J Surg, 2011, 98(2): 268-274. doi: 10.1002/bjs.7305
[3] 王岩, 陶仁海, 曹玉, 等. 预后营养指数在食管腺癌患者预后评估中的价值研究[J]. 中国全科医学, 2016, 19(28): 3428-3433. https://www.cnki.com.cn/Article/CJFDTOTAL-QKYX201628011.htm Wang Y, Tao RH, Cao Y, et al. Investigation in Prognostic Value of Prognostic Nutritional Index in Patients with Esophageal Adenocarcinoma[J]. Zhongguo Quan Ke Yi Xue, 2016, 19(28): 3428-3433. https://www.cnki.com.cn/Article/CJFDTOTAL-QKYX201628011.htm
[4] 中国胸腺肿瘤研究协作组. 胸腺瘤术后临床病理分期与预后相关性的回顾性研究[J]. 中华胸心血管外科杂志, 2017, 33(5): 286-289. Chinese Alliance of Research for Thymomas, ChART. The correlation analysis of thymoma postoperative clinical staging (Masaoka-Koga staging) and prognosis: a retrospective analysis[J]. Zhonghua Xiong Xin Xue Guan Wai Ke Za Zhi, 2017, 33(5): 286-289.
[5] Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients[J]. Nihon Geka Gakkai Zasshi, 1984, 85(9): 1001-1005.
[6] Wang F, Pang L, Fu J, et al. Postoperative survival for patients with thymoma complicating myasthenia gravis-preliminary retrospective results of the ChART database[J]. J Thorac Dis, 2016, 8(4): 711-717. doi: 10.21037/jtd.2016.02.07
[7] Yu L, Zhang XJ, Ma S, et al. Different characteristics of thymomas with and without myasthenia gravis[J]. Ann Surg Oncol, 2012, 19(1): 94-98. doi: 10.1245/s10434-011-1896-8
[8] Zhang Z, Cui Y, Jia R, et al. Myasthenia gravis in patients with thymoma affects survival rate following extended thymectomy[J]. Oncol Lett, 2016, 11(6): 4177-4182. doi: 10.3892/ol.2016.4528
[9] 袁东风, 谷志涛, 梁光辉, 等. 胸腺瘤合并重症肌无力患者预后的临床研究[J]. 中国肺癌杂志, 2018, 21(1): 1-7. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ201801001.htm Yuan DF, Gu ZT, Liang GH, et al. Clinical Study on the Prognosis of Patients with Thymoma with Myasthenia Gravis[J]. Zhongguo Fei Ai Za Zhi, 2018, 21(1): 1-7. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ201801001.htm
[10] 李田, 吴显宁, 解明然, 等. 胸腺切除加前纵隔脂肪清扫治疗重症肌无力的预后分析[J]. 中华外科杂志, 2017, 55(4): 292-296. https://www.cnki.com.cn/Article/CJFDTOTAL-XDZD201905045.htm Li T, Wu XN, Xie MR, et al. Prognostic analysis of patients with myasthenia gravis after extended thymectomy[J]. Zhonghua Wai Ke Za Zhi, 2017, 55(4): 292-296. https://www.cnki.com.cn/Article/CJFDTOTAL-XDZD201905045.htm
[11] 刘洪生, 任海涛, 周立新, 等. 胸腺瘤合并神经系统副肿瘤综合征临床分析[J]. 中华医学杂志, 2017, 97(35): 2770-2774. Liu HS, Ren HT, Zhou LX, et al. Clinical analysis of paraneoplastic neurological syndrome associated with thymoma[J]. Zhonghua Yi Xue Za Zhi, 2017, 97(35): 2770-2774.
[12] 庞烈文, 汪防睿, 方文涛. 重症肌无力对胸腺瘤患者预后的影响[J]. 中华胸心血管外科杂志, 2017, 33(3): 133-134. https://www.cnki.com.cn/Article/CJFDTOTAL-SYZL202004011.htm Pang LW, Wang FR, Fang WT. The influence of myasthenia gravis on the prognosis of thymoma patients[J]. Zhonghua Xiong Xin Xue Guan Wai Ke Za Zhi, 2017, 33(3): 133-134. https://www.cnki.com.cn/Article/CJFDTOTAL-SYZL202004011.htm
[13] 柳阳春, 章晔, 林庆, 等. 重症肌无力胸腺切除围手术期规范、程序化处理探索[J]. 中华胸心血管外科杂志, 2017, 33(3): 151-154. Liu YC, Zhang Y, Lin Q, et al. A protocol for the perioperative management of thymectomy for myasthenia gravis patients[J]. Zhonghua Xiong Xin Xue Guan Wai Ke Za Zhi, 2017, 33(3): 151-154.
[14] 薛志强, 初向阳, 张连斌, 等. 达芬奇机器人与电视胸腔镜治疗胸腺瘤合并重症肌无力的效果[J]. 中华胸心血管外科杂志, 2017, 33(3): 141-143. Xue ZQ, Chu XY, Zhang LB, et al. The study of clinical outcomes of extended thymectomy by robotic and video assisted thoracoscopic surgey for thymoma with myasthenia gravis[J]. Zhonghua Xiong Xin Xue Guan Wai Ke Za Zhi, 2017, 33(3): 141-143.
[15] 杨立, 范翔宇, 陆冬玲, 等. 胸腺瘤239例预后相关因素分析[J]. 中华肿瘤防治杂志, 2016, 23(18): 1264-1267. https://www.cnki.com.cn/Article/CJFDTOTAL-QLZL201618017.htm Yang L, Fan XY, Lu DL, et al. Analysis of factors associated with prognosis of 239 case thymoma[J], Zhonghua Zhong Liu Fang Zhi Za Zhi, 2016, 23(18): 1264-1267. https://www.cnki.com.cn/Article/CJFDTOTAL-QLZL201618017.htm
[16] Wu SJ, Lin YX, Ye H, et al. Lymphocyte to monocyte ratio and prognostic nutritional index predict survival outcomes of hepatitis B virus associated hepatocellular carcinoma patients after curative hepatectomy[J]. J Surg Oncol, 2016, 114(2): 202-210. doi: 10.1002/jso.24297
[17] Kanda MJ, Fujii T, Kodera Y, et al. Nutritional predictors of postoperative outcome in pancreatic cancer[J]. Br J Surg, 2011, 98(2): 268-274. doi: 10.1002/bjs.7305
[18] Wang Y, Liu JF. A retrospective study on the prognostic value of preoperative neutrophil/lymphocyte ratio in patients with primary small-cell carcinoma of the esophagus[J]. Onco Targets Ther, 2017, 10: 2453-2459. doi: 10.2147/OTT.S115637
[19] 张磊, 杨洋, 吴恺, 等. 无症状胸腺瘤患者的CT特征与世界卫生组织分型的关系[J]. 中华实验外科杂志, 2017, 34(1): 140-142. Zhang L, Yang Y, Wu K, et al. Correlation of features of chest computed tomographic scans with histologic subtypes of thymoma according to the World Health Organisation classification in asymptomatic patients[J]. Zhonghua Shi Yan Wai Ke Za Zhi, 2017, 34(1): 140-142.
[20] 张华俊, 程远大, 高阳, 等. 胸腺瘤与胸腺瘤合并重症肌无力患者的临床特点与围手术期临床处理[J]. 中华胸心血管外科杂志, 2017, 33(3): 148-150, 187. Zhang HJ, Cheng YD, Gao Y, et al. Clinical features and experience of perioperative managements of thymomas with and without myasthenia gravis[J]. Zhonghua Xiong Xin Xue Guan Wai Ke Za Zhi, 2017, 33(3): 148-150, 187.
[21] 苏运超, 底锦熙, 笪冀平. 不典型A型胸腺瘤临床病理分析[J]. 中华病理学杂志, 2017, 46(5): 314-317. Su YC, Di JX, Da JP. Clinicopathologic features of atypical type A thymoma[J]. Zhonghua Bing Li Xue Za Zhi, 2017, 46(5): 314-317.
[22] 贾佳, 朱慧军, 王冰, 等. 侵袭性胸腺瘤术后三维适形放疗预后分析[J]. 中华肿瘤防治杂志, 2016, 23(13): 888-892. https://www.cnki.com.cn/Article/CJFDTOTAL-QLZL201613011.htm Jia J, Zhu HJ, Wang B, et al. Analysis for the prognosis of patients with invasive thymoma treated by three-dimensional conformal radiotherapy after operation[J]. Zhonghua Zhong Liu Fang Zhi Za Zhi, 2016, 23(13): 888-892. https://www.cnki.com.cn/Article/CJFDTOTAL-QLZL201613011.htm
[23] 刘乾文, 谷志涛, 杨富, 等. 术后放疗在Ⅰ期/Ⅱ期/Ⅲ期胸腺肿瘤中的作用--ChART回顾性数据库研究结果[J]. 中国肺癌杂志, 2016, 19(7): 465-472. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ201607012.htm Liu QW, Gu ZT, Yang F, et al. Role of Postoperative Radiotherapy for StageⅠ/Ⅱ/Ⅲ Thymic Tumor-Results of the ChART Retrospective Database[J]. Zhongguo Fei Ai Za Zhi, 2016, 19(7): 465-472. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ201607012.htm



 下载:
下载:

