Clinical Characteristics and Prognosis of 123 Patients with Diffuse Large B-cell Lymphoma of Waldeyer’s Ring
-
摘要:目的
探讨原发韦氏环弥漫大B细胞淋巴瘤(Waldeyer’s ring diffuse large B-cell lymphoma, WR-DLBCL)的临床特征、预后因素及治疗策略。
方法回顾性分析天津医科大学肿瘤医院2006年1月至2014年6月收治的123例初治原发韦氏环DLBCL患者,对其临床特征、治疗方式及生存情况比较分析,Kaplan-Meier法计算3、5年生存率,Log rank检验单因素分析,Cox比例风险模型多因素分析。
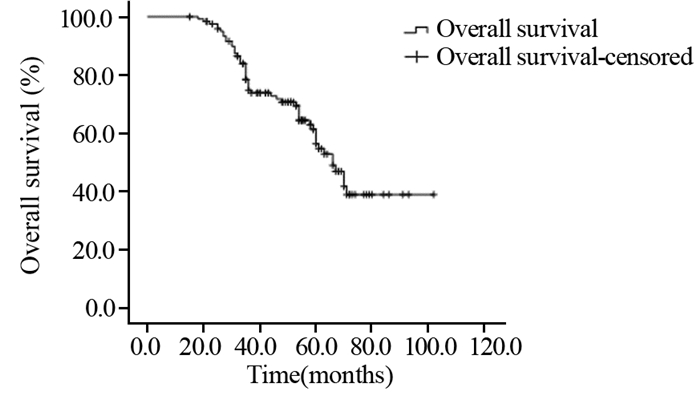
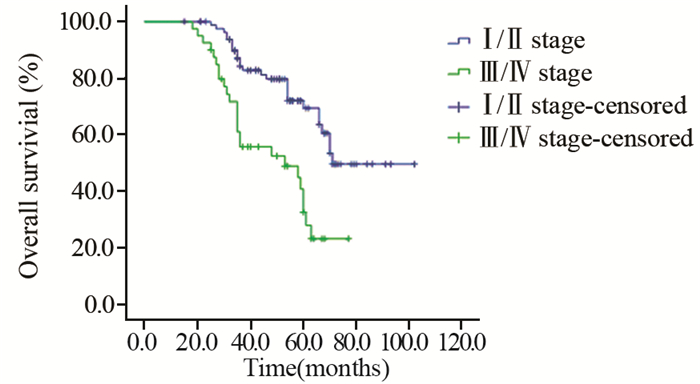
结果123例患者中位年龄为56岁(16~80岁),男72例。Ann Arbor分期:Ⅰ期20 例,Ⅱ期63例,Ⅲ期23例,Ⅳ期17例。中位随访54月,3年和5年生存率分别为74.7%和56.3%,早期(Ⅰ/Ⅱ期)患者3年和5年生存率分别为84.2%和69.4%。单因素分析显示:年龄、体质状况、B症状、临床分期、国际预后指数(IPI)、乳酸脱氢酶(LDH)水平、近期疗效是影响预后的主要因素;多因素分析显示:IPI评分和近期疗效为独立预后因素。
结论原发韦氏环DLBCL多为早期,肿瘤负荷较轻,生存率较高,多数可长期生存。IPI评分和近期疗效是独立预后因素。
-
关键词:
- 环弥漫大B细胞淋巴瘤 /
- 韦氏环 /
- 临床特征 /
- 预后
Abstract:ObjectiveTo investigate the clinical characteristics, prognostic factor and treatment strategy of primary Waldeyer’s ring diffuse large B-cell lymphoma(WR-DLBCL) patients.
MethodsA total of 123 WR-DLBCL patients who were initially diagnosed and treated in Tianjin Medical University Cancer Institute and Hospital from January 2006 to June 2014 were retrospectively analysed, including clinical characteristics, treatment and survival. Kaplan-Meier method was used for evaluating the 3- and 5-year overall survival(OS) rates. Log-rank method was used to evaluate the significance tests. Multivariate analysis was carried out with the Cox proportional hazard model.
ResultsAmong 123 patients, the median age was 56(16-80) years old, including 72 males. Twenty patients were Ann Arbor stageⅠ, 63 patients were stageⅡ, 23 patients were stage Ⅲ, and 17 patients were stage Ⅳ. After a median follow-up of 54 months, the 3- and 5-year OS were 74.7% and 56.3%, and those of stageⅠ-Ⅱwere 84.2% and 69.4%. The univariate analysis revealed that the age, performance status, B symptoms, Ann Arbor stage, international prognostic index (IPI), serum LDH and short-term treatment response were the prognostic factors; multivariate analysis showed that IPI scores and short-term treatment response had significant effects on the prognosis.
ConclusionMost WR-DLBCL patients have stageⅠ-Ⅱdisease and lower tumor burdens, longer survival through chemotherapy and radiotherapy. IPI and short-term treatment response were the independent prognosis factors for WR-DLBCL patients.
-
0 前言
肾细胞癌(renal cell carcinoma, RCC)为泌尿系统三大恶性肿瘤之一,致死率高,预后差[1]。肾透明细胞癌(clear cell renal cell carcinoma, ccRCC)是肾细胞癌最常见的亚型,在发生转移的RCC中占80%~85%,对传统的放疗和化疗均不敏感[2]。目前微创或开放手术切除原发肿瘤仍是治疗ccRCC的最主要方法,但是肾癌患者往往早期无症状,或仅有发热、乏力等全身症状,待出现血尿或肿瘤体积增大压迫其他器官导致肾区疼痛才被发现。此时往往肿瘤体积已较大,或者已发生转移,增加了根治性肾切除术或肾部分切除术的难度。
CD248(tumour endothelial marker 1, TEM-1),又名内皮唾酸蛋白(Endosialin),是近年来发现的一个肿瘤标志物,CD248主要表达于肿瘤细胞与新生血管细胞的内皮细胞表面,是周细胞和成纤维细胞表达的一种间质细胞标志物[3-5],在多种人类恶性肿瘤中高表达,如乳腺癌、卵巢癌、结肠癌、脑癌、肉瘤等,而在正常组织中缺失或低表达[6-10]。然而,到目前为止CD248与肾癌的关系尚无报道。
本研究旨在探讨CD248的表达在人类ccRCC组织中的区域特征、空间分布等信息,将有助于我们进一步了解CD248是否可以作为ccRCC治疗的靶点。
1 资料与方法
1.1 临床资料
收集2011年3月—2016年3月在武汉大学人民医院泌尿外科行原发肾肿瘤切除术的115例患者,均为单侧根治性肾切除,术后明确病理诊断为肾透明细胞癌,同时取17例新鲜标本,及时用液氮冻存备用。患者的肿瘤组织及配对癌旁组织均取自同一标本。临床纳入标准:患者有单侧腰痛或上腹痛、无痛性肉眼血尿等临床症状,或偶然体检时发现并初步诊断为肾占位性病变,通过全腹部CT平扫+增强影像学诊断为肾原发肿瘤,并排除继发于其他器官的转移瘤,所有入组患者需最终病理诊断为肾透明细胞癌。本研究经武汉大学人民医院医学伦理委员会批准。所有患者均签署知情同意书。本研究将ccRCC患者分为CD248高表达组(n=67)和低表达组(n=48)。
1.2 随访
术后随访至2018年12月,随访时间2~72月,随访频率为每两月一次,115例患者中共101例成功随访,14例失访。
1.3 免疫组织化学检测
制作4 μm石蜡切片,根据试剂盒说明书进行免疫组织化学(IHC)分析。设阳性和阴性对照,切片经3%过氧化氢(H2O2)孵育10 min,在暗室中,室温25℃左右以淬灭内源过氧化物酶活性,检测抗原。随后,37℃混合,加一抗(1:200,CD248抗体,美国Invitrogen公司)及原抗(1:50,美国Invitrogen公司)孵育,4℃过夜。室温25℃左右反应15 min,PBS洗涤,加入过氧化物酶,37℃反应40 min,Mayer苏木精对比染色及3′-二氨基联苯胺底物反应。
ccRCC组织的病理学诊断标准:肿瘤细胞的胞质透明或嗜酸性;组织间可见小的薄壁血管组成的网状间隔;一些肿瘤细胞可能呈现为癌巢和腺泡样结构;极少数肿瘤为肉瘤样,巨细胞偶尔可见;少数肿瘤可见坏死、钙化、骨化或纤维黏液化等。CD248染色强度评分定义如下:0分为无染色(−);1~3分为弱阳性(+),黄色或棕黄色;4~6分为中度阳性(++),棕褐色;7~10分为强阳性(+++),褐色或黑褐色。1~6分为低表达组,7~10分为高表达组。结果采用“双盲”法进行评定。
1.4 实时定量聚合酶链反应(qRT-PCR)检测
ABI 7300 RT-PCR系统分析ccRCC及癌旁组织中CD248(NM_020404)mRNA的表达。反转录cDNA按照产品操作说明书进行,反应体系20 μl,包括TB GreenTM Premix Ex TaqTMⅡ(日本TaKaRa)10 μl,上下游引物各0.5 μl(10 pmol/μl)CDNA 2 μl(5 ng/μl),蒸馏水7 μl。qRT-PCR的反应条件为94℃ 5 min预变性,94℃ 45 s,60℃ 60 s,共40个循环。每个样本设3个复孔,ABI 7300系统SDS软件分析mRNA的比值。引物序列为:CD248:5′-TGCGAACACGAATGTGTGGA-3′(上游)和5′-CAATCTGGCACTCATCTGTGTC-(下游),β-actin(内参):5′-GTGGACATCCGCAAAGAC-3′(上游)和5′- AAAGGGTGTAACGCAACTA-3′(下游)。
1.5 统计学方法
所有数据应用SPSS20.0统计软件进行分析,结果以均数±标准差(x±s)表示,单因素方差分析比较各组间差异,两组间比较采用q检验,SPSS20.0软件绘制患者Kaplan-Meier生存曲线,Spearman秩相关分析,并用Log rank检验。P < 0.05为差异有统计学意义,
2 结果
2.1 ccRCC及癌旁组织中CD248的免疫评分及细胞定位
免疫组织化学结果提示在ccRCC组织中,CD248免疫反应平均得分为3.88±0.41,具体得分:3例为-,19例为+,50例为++,43例为+++,共112例阳性,阳性率为97.4%,而癌旁组织(ANCT)的平均得分1.02±0.26,具体得分:68例为-,35例为+,9例为++,3例为+++,共47例阳性,阳性率40.9%,ccRCC组织中的CD248阳性表达免疫组织化学反应强度显著强于癌旁组织,差异有统计学意义(P=0.0061),且CD248蛋白阳性信号定位于细胞核及细胞质,见图 1。
2.2 ccRCC及癌旁组织中CD248 mRNA的表达
CD248 mRNA在癌旁组织中的表达水平明显低于ccRCC组织(1.32±0.29 vs. 3.44±0.32, P=0.0026)。
2.3 CD248表达与ccRCC患者临床病理特征的关系
CD248表达与患者年龄、性别、肾肿瘤TNM分期(参照2017年AJCC第八版指南[2])、肿瘤大小及淋巴结转移均无显著相关性(均P > 0.005),见表 1。
表 1 CD248表达与肾透明细胞癌患者临床病理特征的相关性Table 1 Correlation between CD248 expression and clinicopathological features of ccRCC patients
2.4 CD248蛋白水平与ccRCC患者预后的关系
Kaplan-Meier法生存分析结果显示,CD248低表达组中位生存时间为57.2月,高表达组为44.4月,CD248高表达组OS显著低于CD248低表达组(χ2=5.712, P=0.017),见图 2。
3 讨论
CD248是近年来发现的一个肿瘤标志物,其基因定位于人类11号染色体llql3上,由一种单链跨膜糖蛋白编码,大小为165 kDa。被定义为一种C型凝集素样膜受体,其胞外结构由一个信号序列、一个C型凝集素样结构域、一个寿司状结构域、三个表皮生长因子样结构域和一个糖基化黏蛋白结构域组成,胞内结构为跨膜结构域与细胞质结构域[3-5]。
近年来,国外学者对CD248在肾脏相关疾病中的作用进行了系列研究,Smith等[11]发现CD248主要表达于肾周细胞和肾间质成纤维细胞中,在慢性肾病的肾纤维化过程中发挥重要作用。在人慢性肾病(CKD)标本及小鼠慢性肾纤维化模型中CD248表达明显升高,下调CD248表达能调节肾周细胞和间质细胞的功能,从而抑制肾毛细血管稀疏化和肾间质的纤维化[11-13]。
人类CD248的具体功能目前尚不清楚,动物实验中基因敲除CD248可导致血管、脑部及直结肠肿瘤的生长抑制、侵袭性减弱、血管生成减少等[6-10],因此CD248极有可能通过抗肿瘤血管生成而发挥抗癌作用,并成为潜在的有效治疗靶点,同时也可能适用于肿瘤的早期诊断[14-17]。到目前为止CD248与肾肿瘤的关系尚无文献报道。
本研究首次报告了ccRCC及癌旁组织中CD248的表达差异有统计学意义,ccRCC组织中CD248免疫组织化学免疫强度及阳性率均明显高于癌旁组织,ccRCC组织中CD248 mRNA的表达亦高于癌旁组织。本研究明确了CD248表达与ccRCC的临床病理参数的关系,及其对ccRCC预后的评估价值,由此推测,CD248可能与ccRCC的发生、发展有着密切关系。同时我们还发现CD248的表达与患者性别、年龄、肿瘤TNM分期、肿瘤大小、淋巴结转移并无相关性,但是,Kaplan-Meier生存分析显示,高表达CD248组的ccRCC患者总生存率明显低于低表达组,差异有统计学意义,这些结果表明CD248的表达与ccRCC的发生、发展呈正相关性。但是由于本研究临床样本量有限,CD248在此过程中的具体机制及有哪些信号转导通路参与其中等将在后续作进一步研究。
-
表 1 123例原发韦氏环弥漫大B细胞淋巴瘤患者临床特点与预后因素单因素分析
Table 1 Univariate analysis of relationship between clinical characteristics and survival of 123 WR-DLBCL patients

-
[1] Campo E, Swerdlow SH, Harris NL, et al. The 2008 WHO classification of lymphoid neoplasms and beyond: evolving concepts and practical applications[J]. Blood, 2011, 117(19): 50 19-32. [1] Campo E, Swerdlow SH, Harris NL, et al. The 2008 WHO classification of lymphoid neoplasms and beyond: evolving concepts and practical applications[J]. Blood, 2011, 117(19): 5019-32.
[2] López-Guillermo A, Colomo L, Jiménez M, et al. Diffuse large B-cell lymphoma: clinical and biological characterization and outcome according to the nodal or extranodal primary origin[J]. J Clin Oncol, 2005, 23(12): 2797-804. [2] López-Guillermo A, Colomo L, Jiménez M, et al. Diffuse large B-cell lymphoma: clinical and biological characterization and outcome according to the nodal or extranodal primary origin[J]. J Clin Oncol, 2005, 23(12): 2797-804.
[3] Gutiérrez-García G, Colomo L, Villamor N, et al. Clinicobiological characterization and outcome of primary nodal and extranodal diffuse large B-cell lymphoma in the rituximab era[J]. Leuk Lymphoma, 2010, 51(7): 1225-32. [3] Gutiérrez-García G, Colomo L, Villamor N, et al. Clinicobiological characterization and outcome of primary nodal and extranodal diffuse large B-cell lymphoma in the rituximab era[J]. Leuk Lymphoma, 2010, 51(7): 1225-32.
[4] Laskar S, Mohindra P, Gupta S, et al. Non-Hodgkin lymphoma of the Waldeyer’s ring: clinicopathologic and therapeutic issues[J]. Leuk Lymphoma, 2008, 49(12): 2263-71.
[4] Laskar S, Mohindra P, Gupta S, et al. Non-Hodgkin lymphoma of the Waldeyer’s ring: clinicopathologic and therapeutic issues[J]. Leuk Lymphoma, 2008, 49(12): 2263-71. [5] Ezzat AA, Ibrahim EM, El WA, et al. Localized non-Hodgkin’s lymphoma of Waldeyer’s ring: clinical features, management, and prognosis of 130 adult patients[J]. Head Neck, 2001, 23(7): 547-58.
[5] Ezzat AA, Ibrahim EM, El WA, et al. Localized non-Hodgkin’s lymphoma of Waldeyer’s ring: clinical features, management, and prognosis of 130 adult patients[J]. Head Neck, 2001, 23(7): 54 7-58. [6] Lee SJ, Suh CW, Lee SI, et al. Clinical characteristics, pathological distribution, and prognostic factors in non-Hodgkin lymphoma of Waldeyer’s ring: nationwide Korean study[J]. Korean J Intern Med, 2014, 29(3): 352-60.
[6] Lee SJ, Suh CW, Lee SI, et al. Clinical characteristics, pathological distribution, and prognostic factors in non-Hodgkin lymphoma of Waldeyer’s ring: nationwide Korean study[J]. Korean J Intern Med, 2014, 29(3): 352-60. [7] Laskar S, Mohindra P, Gupta S, et al. Non-Hodgkin lymphoma of the Waldeyer’s ring: clinicopathologic and therapeutic issues[J]. Leuk Lymphoma, 2008, 49(12): 2263-71.
[7] Laskar S, Mohindra P, Gupta S, et al. Non-Hodgkin lymphoma of the Waldeyer’s ring: clinicopathologic and therapeutic issues[J]. Leuk Lymphoma, 2008, 49(12): 2263-71. [8] Qi SN, Li YX, Wang H, et al. Diffuse large B-cell lymphoma: clinical characterization and prognosis of Waldeyer ring versus lymph node presentation[J]. Cancer, 2009, 115(21): 4980-9. [8] Qi SN, Li YX, Wang H, et al. Diffuse large B-cell lymphoma: clinical characterization and prognosis of Waldeyer ring versus lymph node presentation[J]. Cancer, 2009, 115(21): 4980-9.
[9] Li JJ, Hu JP. An analysis of the clinical manifestation and prognosis of 101 cases with non-Hodgkin lymphoma of Waldeyer’s ring[J]. Lin Chuang Xue Ye Xue Za Zhi, 2007, 20(2): 78-80. [励菁菁, 胡 钧培. 咽淋巴环非霍奇金淋巴瘤101例临床及预后分析[J]. 临床 血液学杂志, 2007, 20(2): 78-80.] [9] 励菁菁,胡钧培.咽淋巴环非霍奇金淋巴瘤101例临床及预后分析[J].临床血液学杂志, 2007, 20(2): 78-80. Li JJ, Hu JP. An analysis of the clinical manifestation and prognosis of 101 cases with non-Hodgkin lymphoma of Waldeyer’s ring[J]. Lin Chuang Xue Ye Xue Za Zhi, 2007, 20(2): 78-80.
[10] Hans CP, Weisenburger DD, Greiner TC, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray[J]. Blood, 2004, 10 3(1): 275-82. [10] Hans CP, Weisenburger DD, Greiner TC, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray[J]. Blood, 2004, 103(1): 275-82.
[11] Zhai CW, Wang SY, Epstein-barr virus infection in primary tonsillar diffuse large B cell lymphoma(PTDLBCL) and its clinical significance[J]. Fu Dan Xue Bao(Yi Xue Ban), 2014, 41 (2): 210-5. [翟长文, 王纾宜. EB病毒在原发性扁桃体弥漫大 B细胞淋巴瘤(PTDLBCL)中的表达及其临床意义[J]. 复旦学报 (医学版) , 2014, 41(2): 210-5.] [11] 翟长文,王纾宜. EB病毒在原发性扁桃体弥漫大 B细胞淋巴瘤(PTDLBCL)中的表达及其临床意义[J].复旦学报 (医学版), 2014, 41(2): 210-5. Zhai CW, Wang SY, Epstein-barr virus infection in primary tonsillar diffuse large B cell lymphoma(PTDLBCL) and its clinical significance[J]. Fu Dan Xue Bao(Yi Xue Ban), 2014, 41(2): 210-5.
[12] de Leval L, Bonnet C, Copie-Bergman C, et al. Diffuse large B-cell lymphoma of Waldeyer’s ring has distinct clinicopathologic features: a GELA study[J]. Ann Oncol, 2012, 23(12): 3143-51.
[12] de Leval L, Bonnet C, Copie-Bergman C, et al. Diffuse large B-cell lymphoma of Waldeyer’s ring has distinct clinicopathologic features: a GELA study[J]. Ann Oncol, 2012, 23(12): 3143-51. [13] Laskar S, Bahl G, Muckaden MA, et al. Primary diffuse large B-cell lymphoma of the tonsil: is a higher radiotherapy dose required?[J]. Cancer, 2007, 110(4): 816-23. [13] Laskar S, Bahl G, Muckaden MA, et al. Primary diffuse large B-cell lymphoma of the tonsil: is a higher radiotherapy dose required?[J]. Cancer, 2007, 110(4): 816-23.
[14] Mian M, Ferreri AJ, Rossi A, et al. Role of radiotherapy in patients with early-stage diffuse large B-cell lymphoma of Waldeyer’s ring in remission after anthracycline-containing chemotherapy[J]. Leuk Lymphoma, 2013, 54(1): 62-8.
[14] Mian M, Ferreri AJ, Rossi A, et al. Role of radiotherapy in patients with early-stage diffuse large B-cell lymphoma of Waldeyer’s ring in remission after anthracycline-containing chemotherapy[J]. Leuk Lymphoma, 2013, 54(1): 62-8. [15] Guo R, Qian LT, Zhang HY, et al. Outcome and prognostic factors in patients with Waldeyer’s ring non-Hodgkin lymphoma[J]. Zhonghua Zhong Liu Fang Zhi Za Zhi, 2012, 19(10): 780-2. [郭蕊, 钱立庭, 张红雁, 等. 韦氏环非霍奇金淋巴瘤综合治疗疗效及其 预后因素分析[J]. 中华肿瘤防治杂志, 2012, 19(10): 780-2.] [15] 郭蕊,钱立庭,张红雁,等.韦氏环非霍奇金淋巴瘤综合治疗疗效及其预后因素分析[J].中华肿瘤防治杂志, 2012, 19(10): 780-2. Guo R, Qian LT, Zhang HY, et al. Outcome and prognostic factors in patients with Waldeyer’s ring non-Hodgkin lymphoma[J]. Zhonghua Zhong Liu Fang Zhi Za Zhi, 2012, 19(10): 780-2.
[16] Qin Y, Shi YK, He XH, et al. Clinical Features of 89 Patients with Primary Non-Hodgkin Lymphoma of the Tonsil[J]. Ai Zheng, 20 06, 25(4): 481-5. [秦燕, 石远凯, 何小慧, 等. 原发扁桃体非霍 奇金淋巴瘤89例临床分析[J]. 癌症, 2006, 25(4): 481-5.] [16] 秦燕,石远凯,何小慧,等.原发扁桃体非霍奇金淋巴瘤89例临床分析[J].癌症, 2006, 25(4): 481-5. Qin Y, Shi YK, He XH, et al. Clinical Features of 89 Patients with Primary Non-Hodgkin Lymphoma of the Tonsil[J]. Ai Zheng, 2006, 25(4): 481-5.
[17] 汤忠祝,马胜林,朱远,等.韦氏环恶性淋巴瘤不同放化疗疗效分析[J].肿瘤学杂志, 2002, (6): 360-1. Tang ZZ, Ma SL, Zhu Y, et al. An analysis of the treatment efficacy of different radiotherapy and chemotherapy methods in patients with malignant lymphoma of Waldeyer’s Ring[J]. Zhong Liu Xue Za Zhi, 2002, (6): 360-1.
[17] Tang ZZ, Ma SL, Zhu Y, et al. An analysis of the treatment efficacy of different radiotherapy and chemotherapy methods in patients with malignant lymphoma of Waldeyer’s Ring[J]. Zhong Liu Xue Za Zhi, 2002, (6): 360-1. [汤忠祝, 马胜林, 朱远, 等. 韦 氏环恶性淋巴瘤不同放化疗疗效分析[J]. 肿瘤学杂志, 2002, (6) : 360-1.] [18] Zhang K, Li ML, Yu XL, et al. Testicular diffuse large B cell lymphoma with colorectal cancer: one case report[J]. Zhong Liu Fang Zhi Yan Jiu, 2014, 41(7): 859-60. [张克, 李美林, 于晓丽, 等. 睾丸原发弥漫大B细胞淋巴瘤伴直肠癌1例[J]. 肿瘤防治研 究, 2014, 41(7): 859-60. ] [18] 张克,李美林,于晓丽,等.睾丸原发弥漫大B细胞淋巴瘤伴直肠癌1例[J].肿瘤防治研究, 2014, 41(7): 859-60. Zhang K, Li ML, Yu XL, et al. Testicular diffuse large B cell lymphoma with colorectal cancer: one case report[J]. Zhong Liu Fang Zhi Yan Jiu, 2014, 41(7): 859-60.
[19] Coiffier B, Thieblemont C, Van Den Neste E, et al. Longterm outcome of patients in the LNH-98.5 trial, the first randomized study comparing rituximab-CHOP to standard CHOP chemotherapy in DLBCL patients: a study by the Groupe d’Etudes des Lymphomes de l’Adulte[J]. Blood, 2010, 116(12): 2040-5.
[19] Coiffier B, Thieblemont C, Van Den Neste E, et al. Longterm outcome of patients in the LNH-98.5 trial, the first randomized study comparing rituximab-CHOP to standard CHOP chemotherapy in DLBCL patients: a study by the Groupe d’Etudes des Lymphomes de l’Adulte[J]. Blood, 2010, 116(12): 2040-5. [20] Chang DT, Mendenhall NP, Lynch JW, et al. Long-term outcomes for stageⅠ-Ⅱ aggressive non-Hodgkin lymphoma of Waldeyer’s ring[J]. Am J Clin Oncol, 2009, 32(3): 233-7. [20] Chang DT, Mendenhall NP, Lynch JW, et al. Long-term outcomes for stageⅠ-Ⅱ aggressive non-Hodgkin lymphoma of Waldeyer’s ring[J]. Am J Clin Oncol, 2009, 32(3): 233-7.
[21] Wilder RB, Rodriguez MA, Medeiros LJ, et al. International prognostic index-based outcomes for diffuse large B-cell lymphomas[J]. Cancer, 2002, 94(12): 3083-8.
[21] Wilder RB, Rodriguez MA, Medeiros LJ, et al. International prognostic index-based outcomes for diffuse large B-cell lymphomas[J]. Cancer, 2002, 94(12): 3083-8. [22] Li YX, Gao YH, Yuan ZY, et al. Prognostic significance of international prognostic index in non-Hodgkin’ s lymphoma of Waldeyer’s ring[J]. Zhonghua Fang She Zhong Liu Xue Za Zhi, 20 02, 11(2): 105-10. [李晔雄, 高远红, 袁智勇, 等. 国际预后指 数在韦氏环非霍奇金淋巴瘤的预后意义[J]. 中华放射肿瘤学杂 志, 2002, 11(2): 105-10.] [22] 李晔雄,高远红,袁智勇,等.国际预后指数在韦氏环非霍奇金淋巴瘤的预后意义[J].中华放射肿瘤学杂志, 2002, 11(2): 105-10. Li YX, Gao YH, Yuan ZY, et al. Prognostic significance of international prognostic index in non-Hodgkin’ s lymphoma of Waldeyer’s ring[J]. Zhonghua Fang She Zhong Liu Xue Za Zhi, 2002, 11(2): 105-10.




 下载:
下载: