Prognostic Analysis of Socioeconomic Factors in Multiple Myeloma Patients and Construction of A Myeloma-specific Survival Prediction Model
-
摘要:目的
探究社会经济学因素对多发性骨髓瘤(MM)患者预后的影响并构建预测模型评估患者骨髓瘤特异性生存(MSS)。
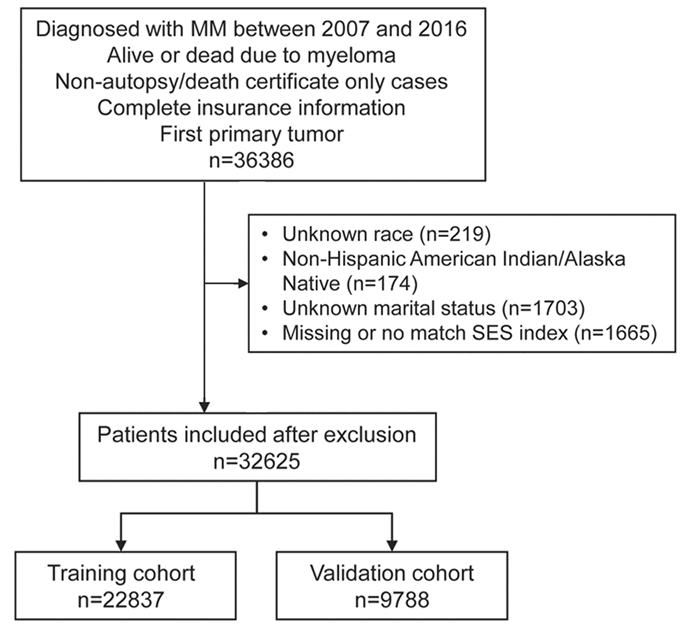
方法由SEER数据库纳入32 625例2007年1月至2016年12月间诊断为MM的患者。Cox回归模型分析MSS的预测因素,森林图展现多因素亚组分析的结果,多因素Cox分析中确定的显著变量用来构建列线图。曲线下面积(AUC)和校准图评估列线图的预测性能,利用限制性三次样条曲线构建基于列线图评分的风险分层系统。
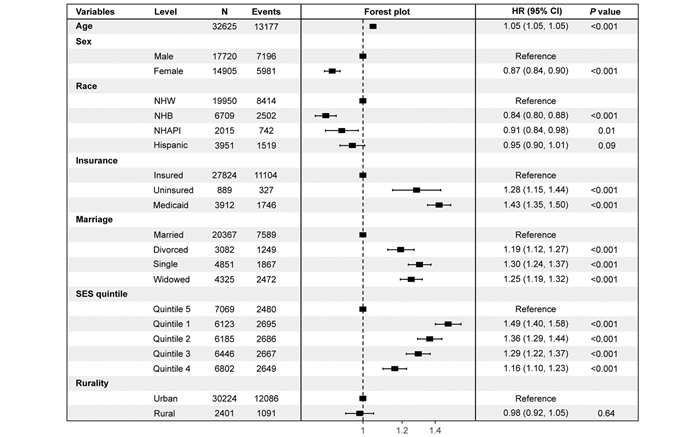
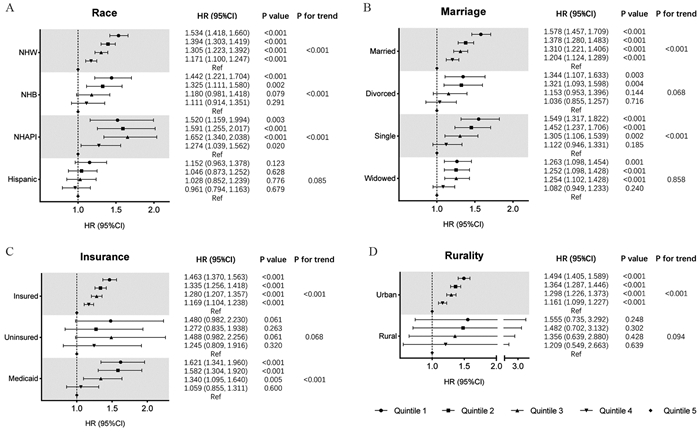
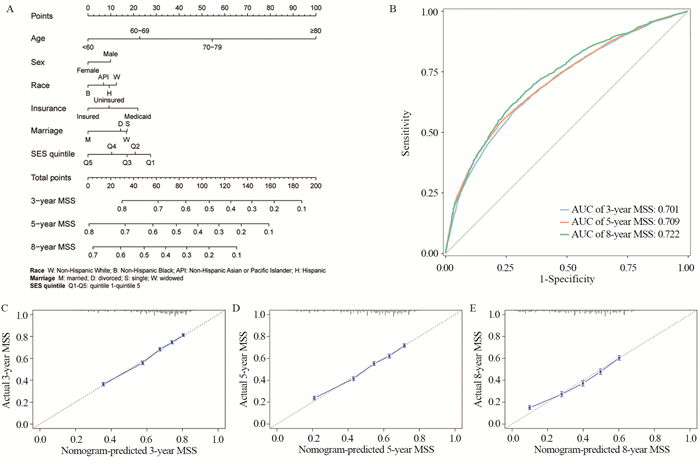
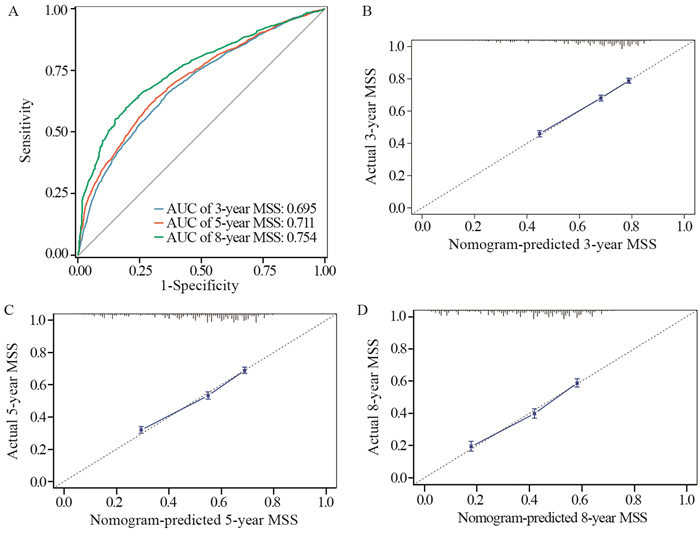
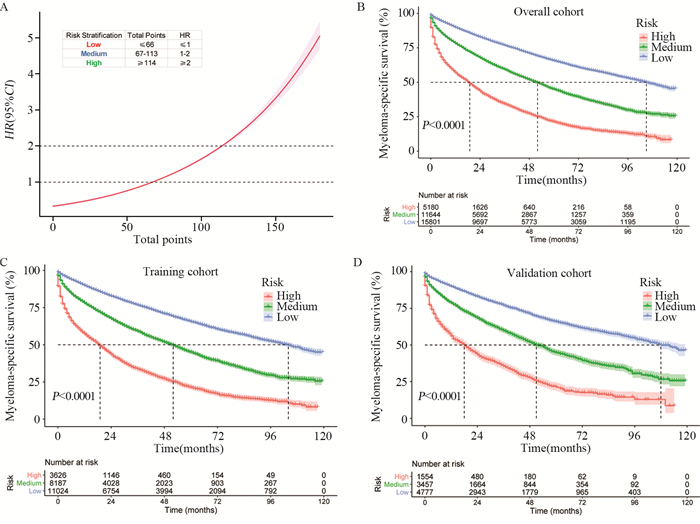
结果患者按其社会经济地位(SES)的高低分为五组,SES更高的群体中白人、有保险者、已婚人群和城市居民的比例相对更高。单因素及多因素Cox分析表明年龄、性别、种族、婚姻状态、保险状况和SES是患者MSS独立预后影响因素(均P < 0.001)。亚组分析显示随着SES降低,MSS风险增加的线性趋势在白人、已婚、有保险和城市患者中最为显著(均P < 0.001)。构建的列线图在训练集和验证集中均展现出良好的区分度和准确性,其预测3年、5年和8年MSS的AUC值分别为0.701、0.709和0.722。根据列线图总分和风险比建立了风险分层模型,所划分的三类不同风险等级组别间存在显著的生存差异(均P < 0.001)。
结论社会经济学因素如婚姻状态、保险状况和SES等能够对MM患者的生存结局造成明显影响,基于这些因素构建的列线图及风险分层模型能较准确可靠地预测MSS。
Abstract:ObjectiveTo investigate the effects of socioeconomic factors on the prognosis of multiple myeloma (MM) patients and construct a prediction model for evaluating myeloma-specific survival (MSS) rates.
MethodsA total of 32625 patients diagnosed with MM between January 2007 and December 2016 were included through the SEER database. Cox regression model was used to analyze the predictive indicators of MSS. The results of the multivariate subgroup analysis were presented as forest plots. The significant factors identified in the multivariate Cox analysis were used to construct a nomogram. The predictive performance of the nomogram was assessed using the AUC and calibration plots. A nomogram score-based risk stratification system was constructed using a restricted cubic spline.
ResultsPatients were divided into five groups according to their socioeconomic status (SES). Groups with higher SES had relatively higher proportions of those part of the White, insured, married, and urban populations. Age, gender, race, marital status, insurance status, and SES were independent prognostic factors of MSS (all P < 0.001). The linear trend of increased MSS risk with decreasing SES was most pronounced among the White, married, insured, and urban patients (all P < 0.001). The nomogram exhibited good discrimination and accuracy in both training and validation sets, showing AUC values of 0.701, 0.709, and 0.722 for predicting 3-, 5-, and 8-year MSS, respectively. A risk stratification model was established based on the nomogram total points and the HR, which then divided patients into three different risk levels with substantial survival disparities (all P < 0.001).
ConclusionSocioeconomic factors, such as marital status, insurance status, and SES, have a significant impact on the survival outcomes of MM patients. The nomogram and the risk stratification model based on these factors can accurately and reliably predict MSS.
-
Key words:
- Multiple myeloma /
- Socioeconomic factors /
- Myeloma-specific survival /
- Prediction model
-
Competing interests: The authors declare that they have no competing interests.利益冲突声明:所有作者均声明不存在利益冲突。作者贡献:徐嘉轩:研究设计、数据分析及论文撰写左依凡、孙晶晶:文献查阅、资料收集陈兵:论文指导及修改
-
表 1 多发性骨髓瘤(MM)患者的基线特征
Table 1 Baseline characteristics of multiple myeloma(MM) patients

表 2 MM患者骨髓瘤特异性生存的单因素Cox分析
Table 2 Univariate Cox analysis of myeloma-specific survival of MM patients

-
[1] Kumar SK, Rajkumar V, Kyle RA, et al. Multiple myeloma[J]. Nat Rev Dis Primers, 2017, 3: 17046. doi: 10.1038/nrdp.2017.46
[2] Liu J, Liu W, Mi L, et al. Incidence and mortality of multiple myeloma in China, 2006-2016: an analysis of the Global Burden of Disease Study 2016[J]. J Hematol Oncol, 2019, 12(1): 136. doi: 10.1186/s13045-019-0807-5
[3] Pulte D, Jansen L, Brenner H. Changes in long term survival after diagnosis with common hematologic malignancies in the early 21st century[J]. Blood Cancer J, 2020, 10(5): 56. doi: 10.1038/s41408-020-0323-4
[4] Fonseca R, Abouzaid S, Bonafede M, et al. Trends in overall survival and costs of multiple myeloma, 2000-2014[J]. Leukemia, 2017, 31(9): 1915-1921. doi: 10.1038/leu.2016.380
[5] Sun T, Wang S, Sun H, et al. Improved survival in multiple myeloma, with a diminishing racial gap and a widening socioeconomic status gap over three decades[J]. Leuk Lymphoma, 2018, 59(1): 49-58. doi: 10.1080/10428194.2017.1335398
[6] Costa LJ, Brill IK, Brown EE. Impact of marital status, insurance status, income, and race/ethnicity on the survival of younger patients diagnosed with multiple myeloma in the United States[J]. Cancer, 2016, 122(20): 3183-3190. doi: 10.1002/cncr.30183
[7] Fiala MA, Finney JD, Liu J, et al. Socioeconomic status is independently associated with overall survival in patients with multiple myeloma[J]. Leuk Lymphoma, 2015, 56(9): 2643-2649. doi: 10.3109/10428194.2015.1011156
[8] Makhani SS, Shively D, Castro G, et al. Association of insurance disparities and survival in adults with multiple myeloma: A non-concurrent cohort study[J]. Leuk Res, 2021, 104: 106542. doi: 10.1016/j.leukres.2021.106542
[9] Tang L, Pan Z, Zhang X. The effect of marital status on the survival of patients with multiple myeloma[J]. Hematology, 2022, 27(1): 187-197. doi: 10.1080/16078454.2022.2026027
[10] Intzes S, Symeonidou M, Zagoridis K, et al. Socioeconomic Status Is an Independent Prognostic Factor for Overall Survival in Patients With Multiple Myeloma: Real-World Data From a Cohort of 223 Patients[J]. Clin Lymphoma Myeloma Leuk, 2020, 20(10): 704-711. doi: 10.1016/j.clml.2020.05.013
[11] Castañeda-Avila MA, Jesdale BM, Beccia A, et al. Differences in survival among multiple myeloma patients in the United States SEER population by neighborhood socioeconomic status and race/ethnicity[J]. Cancer Causes Control, 2021, 32(9): 1021-1028. doi: 10.1007/s10552-021-01454-w
[12] Chamoun K, Firoozmand A, Caimi P, et al. Socioeconomic Factors and Survival of Multiple Myeloma Patients[J]. Cancers (Basel), 2021, 13(4): 590. doi: 10.3390/cancers13040590
[13] Intzes S, Symeonidou M, Zagoridis K, et al. Socioeconomic Status is Globally a Prognostic Factor for Overall Survival of Multiple Myeloma Patients: Synthesis of Studies and Review of the Literature[J]. Mediterr J Hematol Infect Dis, 2021, 13(1): e2021006.
[14] Collins GS, Reitsma JB, Altman DG, et al. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): the TRIPOD statement[J]. Ann Intern Med, 2015, 162(1): 55-63. doi: 10.7326/M14-0697
[15] Harwood M, Dunn N, Moore J, et al. Trends in myeloma relative survival in Queensland by treatment era, age, place of residence, and socioeconomic status[J]. Leuk Lymphoma, 2020, 61(3): 721-727. doi: 10.1080/10428194.2019.1688322
[16] Yu M, Tatalovich Z, Gibson JT, et al. Using a composite index of socioeconomic status to investigate health disparities while protecting the confidentiality of cancer registry data[J]. Cancer Causes Control, 2014, 25(1): 81-92. doi: 10.1007/s10552-013-0310-1
[17] Xu L, Wang X, Pan X, et al. Education level as a predictor of survival in patients with multiple myeloma[J]. BMC Cancer, 2020, 20(1): 737. doi: 10.1186/s12885-020-07178-5
[18] Boen CE, Barrow DA, Bensen JT, et al. Social Relationships, Inflammation, and Cancer Survival[J]. Cancer Epidemiol Biomarkers Prev, 2018, 27(5): 541-549. doi: 10.1158/1055-9965.EPI-17-0836
[19] Freeman A, Tyrovolas S, Koyanagi A, et al. The role of socio-economic status in depression: results from the COURAGE (aging survey in Europe)[J]. BMC Public Health, 2016, 16(1): 1098. doi: 10.1186/s12889-016-3638-0
[20] Bortolato B, Hyphantis TN, Valpione S, et al. Depression in cancer: The many biobehavioral pathways driving tumor progression[J]. Cancer Treat Rev, 2017, 52: 58-70. doi: 10.1016/j.ctrv.2016.11.004
[21] Kruk J, Aboul-Enein BH, Bernstein J, et al. Psychological Stress and Cellular Aging in Cancer A Meta-Analysis[J]. Oxid Med Cell Longev, 2019, 2019: 1270397.



 下载:
下载: