Correlation of Systemic Immune Inflammatory Index and Tumor Markers with Bone Metastasis of Lung Cancer
-
摘要:目的
评估肺癌患者治疗前系统免疫炎症指数(SII)、肺癌肿瘤标志物CEA、Cyfra21-1、NSE对肺癌骨转移的预测及诊断价值。
方法回顾性分析618例肺癌患者临床资料,根据基线时是否骨转移,对诊断组(基线时已经发生骨转移患者和随访未发生骨转移患者)与预测组(随访发生骨转移患者与随访未发生骨转移患者)进行数据分析,确定上述指标与肺癌骨转移的相关性。
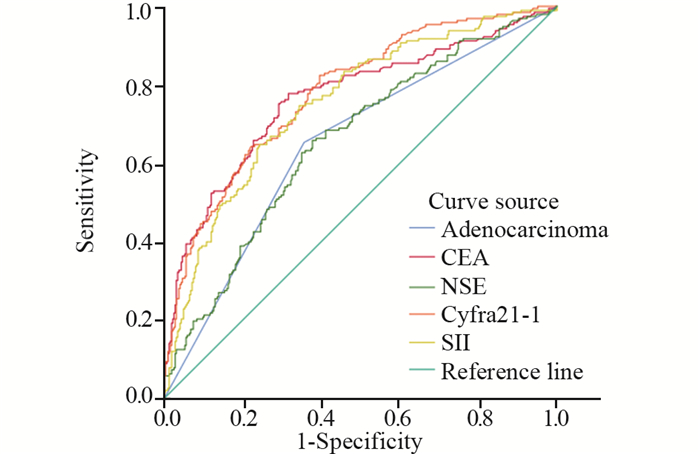
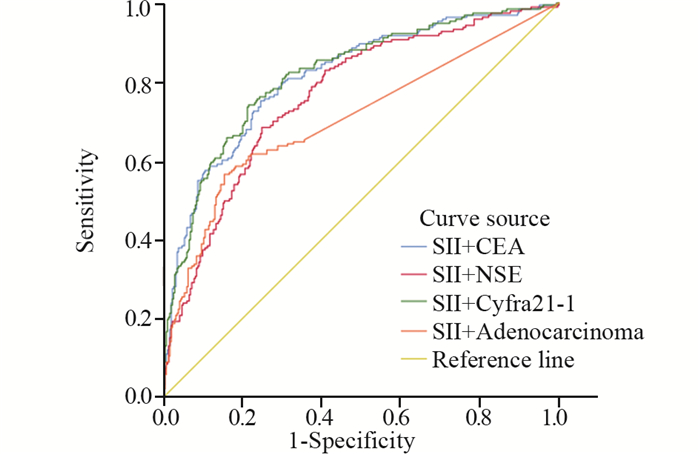
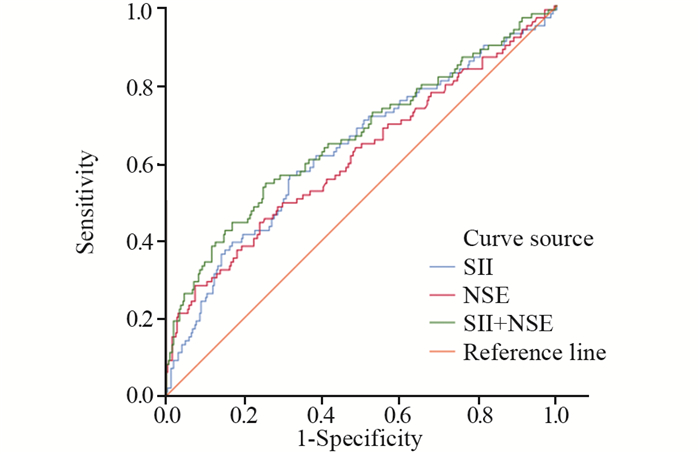
结果预测组:Logistic单因素分析显示SII≥850、NSE≥58.64 ng/ml是肺癌骨转移的独立危险因素和独立预测因素。SII+NSE组合模型曲线下面积为0.662,敏感度为54.5%,特异性为74.5%,优于单一因素预测价值(95%CI: 0.596-0.728, P < 0.001)。诊断组:Logistic回归分析结果显示肺腺癌、SII≥951.6、CEA≥5.14 ng/ml、NSE≥20.15 ng/ml、Cyfra21-1≥3.94 ng/ml是肺癌患者发生骨转移的独立危险因素(P < 0.05),SII单独诊断肺癌骨转移的曲线下面积为0.754,SII+Cyfra21-1组合模型曲线下面积最大,AUC为0.82,敏感度为74%,特异性为78.5%,并优于任何单因素曲线下面积(P < 0.05)。
结论SII、CEA、Cyfra21-1、NSE在骨转移组水平均显著高于非骨转移组,当SII联合其他单一危险因素时,预测价值及诊断价值进一步提高。
Abstract:ObjectiveTo evaluate the value of the systemic immune-inflammatory index (SII), CEA, Cyfra21-1, and NSE in predicting and diagnosing bone metastasis of lung cancer.
MethodsThe clinical data of 618 patients with lung cancer were retrospectively analyzed. According to the bone metastasis at baseline, the data of the diagnosis group (patients with bone metastasis at baseline and patients without bone metastasis during follow-up) and the prediction group (patients with bone metastasis during follow-up and patients without bone metastasis during follow-up) were analyzed to determine the correlation between the above indicators and lung cancer bone metastasis.
ResultsPredictive group: SII≥850 and NSE≥58.64 ng/ml were independent risk factors and independent predictors for lung cancer bone metastasis. The AUC of the combined SII+NSE model was 0.662, with a sensitivity of 54.5% and a specificity of 74.5%; it was superior to the predictive value of single factor (95%CI: 0.596-0.728; P < 0.001). Diagnostic group: lung adenocarcinoma, SII≥951.6, CEA≥5.14 ng/ml, NSE≥20.15 ng/ml, and Cyfra21-1≥3.94 ng/ml were independent risk factors for bone metastasis in lung cancer patients (P < 0.05). The AUC of SII alone in the diagnosis of lung cancer bone metastasis was 0.754. The AUC of the SII+Cyfra21-1 combined model was 0.82 which was the largest, with a sensitivity of 74% and a specificity of 78.5%; it was superior to any univariate AUC (P < 0.05).
ConclusionThe levels of SII, CEA, Cyfra21-1, and NSE in the bone metastasis group are significantly higher than those in the non-bone metastasis group. The predictive and diabnostic values would be improved further when SII combined with other single risk factors.
-
Key words:
- Lung cancer /
- Bone metastasis /
- Systemic immune-inflammatory index /
- Risk factors /
- Tumor marker
-
Competing interests: The authors declare that they have no competing interests.作者贡献:唐敏:选题设计、病例资料与数据收集、文章撰写和修改李桂香:指导选题与设计、文章修改
-
表 1 预测组肺癌患者的临床特征
Table 1 Clinical characteristics of lung cancer patients in the predictive group

表 2 预测组肺癌患者实验室检查资料及特征
Table 2 Laboratory data and characteristics of patients with lung cancer

表 3 预测组肺癌骨转移危险因素Logistic单因素及多因素分析结果
Table 3 Results of Logistic univariate and multivariate analyses of risk factors of bone metastasis of lung cancer in the predictive group

表 4 肺癌骨转移炎性反应指标预测效能评估
Table 4 Evaluation of predictive efficacy of inflammatory markers for bone metastasis of lung cancer

表 5 诊断组肺癌患者临床特征
Table 5 Basic clinical data and characteristics of patients with lung cancer in the diagnosis group

表 6 诊断组肺癌患者炎性反应指标对比(M(P25, P75)
Table 6 Comparison of inflammatory parameters in patients with lung cancer in the diagnosis group (M(P25, P75)

表 7 诊断组肺癌骨转移危险因素Logistic单因素及多因素分析
Table 7 Results of Logistic univariate and multivariate analyses of risk factors of bone metastasis of lung cancer in the diagnosis group

表 8 肺癌骨转移相关危险因素诊断效能评估
Table 8 Evaluation of diagnostic efficacy of risk factors related to bone metastasis of lung cancer

-
[1] Hong S, Youk T, Lee SJ, et al. Bone metastasis and skeletal-related events in patients with solid cancer: A Korean nationwide health insurance database study[J]. PLoS One, 2020, 15(7): e0234927. doi: 10.1371/journal.pone.0234927
[2] 董智, 赵军, 柳晨, 等. 肺癌骨转移诊疗专家共识(2019版)[J]. 中国肺癌杂志, 2019, 22(4): 187-207. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ201904001.htm Dong Z, Zhao J, Liu C, et al. Expert Consensus on Diagnosis and Treatment of Bone Metastasis from Lung Cancer (2019 Edition)[J]. Zhongguo Fei Ai Za Zhi, 2019, 22 (4): 187-207. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ201904001.htm
[3] Niu Y, Lin Y, Pang H, et al. Risk factors for bone metastasis in patients with primary lung cancer: A systematic review[J]. Medicine (Baltimore), 2019, 98(3): e14084. doi: 10.1097/MD.0000000000014084
[4] Wu XT, Zhou JW, Pan LC, et al. Clinical features and prognostic factors in patients with bone metastases from non-small cell lung cancer[J]. J Int Med Res, 2020, 48(5): 300060520925644.
[5] Chai X, Yinwang E, Wang Z, et al. Predictive and Prognostic Biomarkers for Lung Cancer Bone Metastasis and Their Therapeutic Value[J]. Front Oncol, 2021, 11: 692788. doi: 10.3389/fonc.2021.692788
[6] Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow?[J]. Lancet, 2001, 357(9255): 539-545. doi: 10.1016/S0140-6736(00)04046-0
[7] Mirili C, Guney IB, Paydas S, et al. Prognostic significance of neutrophil/lymphocyte ratio (NLR) and correlation with PET-CT metabolic parameters in small cell lung cancer (SCLC)[J]. Int J Clin Oncol, 2019, 24(2): 168-178. doi: 10.1007/s10147-018-1338-8
[8] Chen JL, Wu JN, Lv XD, et al. The value of red blood cell distribution width, neutrophil-to-lymphocyte ratio, and hemoglobin-to-red blood cell distribution width ratio in the progression of non-small cell lung cancer[J]. PLoS One, 2020, 15(8): e0237947. doi: 10.1371/journal.pone.0237947
[9] Yan X, Li G. Preoperative systemic immune-inflammation index predicts prognosis and guides clinical treatment in patients with non-small cell lung cancer[J]. Biosci Rep, 2020, 40(3): BSR20200352. doi: 10.1042/BSR20200352
[10] Mandaliya H, Jones M, Oldmeadow C, et al. Prognostic biomarkers in stage Ⅳ non-small cell lung cancer (NSCLC): neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR) and advanced lung cancer inflammation index (ALI)[J]. Transl Lung Cancer Res, 2019, 8(6): 886-894. doi: 10.21037/tlcr.2019.11.16
[11] Graziano V, Grassadonia A, Iezzi L, et al. Combination of peripheral neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio is predictive of pathological complete response after neoadjuvant chemotherapy in breast cancer patients[J]. Breast, 2019, 44: 33-38. doi: 10.1016/j.breast.2018.12.014
[12] Kobayashi S, Karube Y, Inoue T, et al. Advanced Lung Cancer Inflammation Index Predicts Outcomes of Patients with Pathological Stage IA Lung Adenocarcinoma Following Surgical Resection[J]. Ann Thorac Cardiovasc Surg, 2019, 25(2): 87-94. doi: 10.5761/atcs.oa.18-00158
[13] da Silva GT, Bergmann A, Thuler LCS. Incidence and Risk Factors for Bone Metastasis in Non-Small Cell Lung Cancer[J]. Asian Pac J Cancer Prev, 2019, 20(1): 45-51. doi: 10.31557/APJCP.2019.20.1.45
[14] Wang H, Zhang Y, Zhu H, et al. Risk factors for bone metastasis in completely resected non-small-cell lung cancer[J]. Future Oncol, 2017, 13(8): 695-704. doi: 10.2217/fon-2016-0237
[15] 姚源山, 周银杰, 杨振华, 等. 非小细胞肺癌患者术后发生骨转移的危险因素[J]. 中国肺癌杂志, 2018, 21(6): 476-480. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ201806010.htm Yao YS, Zhou YJ, Yang ZH, et al. [Risk Factors of Non-small Cell Lung Cancer with Bone Metastasis after Therapy][J]. Zhongguo Fei Ai Za Zhi, 2018, 21(6): 476-480. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ201806010.htm
[16] Sun JM, Ahn JS, Lee S, et al. Predictors of skeletal-related events in non-small cell lung cancer patients with bone metastases[J]. Lung Cancer, 2011, 71(1): 89-93. doi: 10.1016/j.lungcan.2010.04.003
[17] Zhou Y, Yu QF, Peng AF, et al. The risk factors of bone metastases in patients with lung cancer[J]. Sci Rep, 2017, 7(1): 89701.
[18] Wang B, Chen L, Huang C, et al. The homogeneous and heterogeneous risk factors for occurrence and prognosis in lung cancer patients with bone metastasis[J]. J Bone Oncol, 2019, 17: 100251. doi: 10.1016/j.jbo.2019.100251
[19] Gao Y, Zhang H, Li Y, et al. Preoperative increased systemic immune-inflammation index predicts poor prognosis in patients with operable non-small cell lung cancer[J]. Clin Chim Acta, 2018, 484: 272-277. doi: 10.1016/j.cca.2018.05.059
[20] Wang Y, Li Y, Chen P, et al. Prognostic value of the pretreatment systemic immune-inflammation index (SⅡ) in patients with non-small cell lung cancer: a meta-analysis[J]. Ann Transl Med, 2019, 7(18): 433. doi: 10.21037/atm.2019.08.116
[21] Numata T, Endo T, Yanai H, et al. Serum CEA and CYFRA Levels in ALK-rearranged NSCLC Patients: Correlation With Distant Metastasis[J]. In Vivo, 2020, 34(4): 2095-2100. doi: 10.21873/invivo.12013
[22] 赵婉婷, 庄岳鹏, 敖海燕. BALP、CA125和NSE在肺癌骨转移诊断和疗效评价中的价值[J]. 肿瘤学杂志, 2019, 25(11): 1016-1018. doi: 10.11735/j.issn.1671-170X.2019.11.B018 Zhao WT, Zhuang YP, Ao HY. The Value of Diagnosis and Effect Evaluation of BALP, CA125 and NSE in Lung Cancer Bone Metastasis[J]. Zhong Liu Xue Za Zhi, 2019, 25 (11): 1016-1018. doi: 10.11735/j.issn.1671-170X.2019.11.B018
[23] Ren X, Zhang Y, Lyu Y, et al. Lactate dehydrogenase and serum tumor markers for predicting metastatic status in geriatric patients with lung adenocarcinoma[J]. Cancer Biomark, 2019, 26(2): 139-150. doi: 10.3233/CBM-190201



 下载:
下载: