-
摘要:
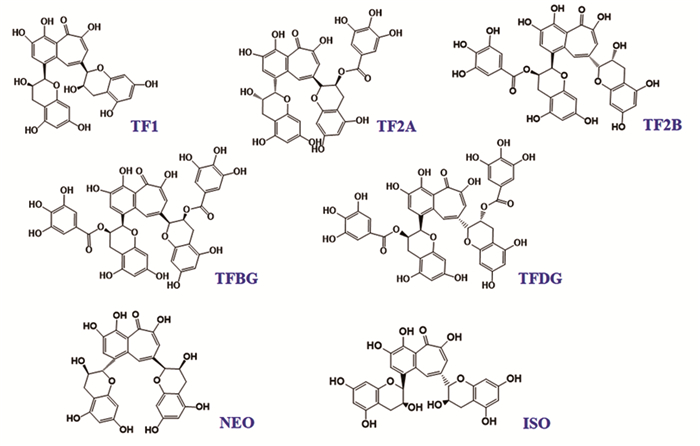
茶黄素类(Theaflavins)是从红茶或绿茶中提取的一类天然产物,在胃癌、肝癌及乳腺癌等多种肿瘤中具有显著的抗肿瘤效果,一度被认为是癌症新药研发的新方向。但是茶黄素抗肿瘤的机制涉及多种生物学过程,且调控复杂。因此,本文就茶黄素在促进肿瘤细胞凋亡、诱导肿瘤细胞有丝分裂阻滞和调节肿瘤免疫过程中的作用展开综述,并概述了茶黄素通过MAPK、PI3K/AKT、Hedgehog、NF-κB、JAK/STAT及Wnt/β-Catenin等信号通路抑制肿瘤发生和生长的机制,以期为癌症治疗及抗癌药物研发提供新的思路。
Abstract:Theaflavins are a class of natural products extracted from black tea or green tea, with significant anti-tumor effects on gastric cancer, liver cancer, breast cancer and other tumors. Theaflavins were once considered as the new products for anticancer therapy. However, the anti-tumor mechanism of theaflavins involves a variety of biological processes, and the regulation is complex. Therefore, this article summarizes the role of theaflavins in promoting tumor cell apoptosis, inducing tumor cell mitotic arrest and regulating tumor immunity, and reviews the inhibition of tumorigenesis and growth through MAPK, PI3K/AKT, Hedgehog, NF-κB, JAK/STAT and Wnt/β-Catenin signal pathways, in order to provide new ideas for cancer treatment and anti-cancer drug development.
-
Key words:
- Theaflavins /
- Signal path /
- Anticancer /
- Mechanism
-
0 引言
维布妥昔单抗(brentuximab vedotin, BV)是一种新型的靶向抗体-药物偶联物(ADC),其由靶向CD30的单克隆抗体和抗有丝分裂药物单甲基澳瑞他汀E(monomethyl auristatin E, MMAE)共价连接而形成。当药物与胞膜上的CD30相结合后,MMAE被释放到细胞质中,随后与微管结合,使细胞阻滞在有丝分裂准备期/有丝分裂期(G2/M),从而诱导其凋亡发生[1]。BV已被国内批准用于CD30阳性的复发或难治性原发性皮肤间变性大细胞淋巴瘤(pcALCL)、系统性间变性大细胞淋巴瘤(sALCL)以及复发或难治性经典型霍奇金淋巴瘤(cHL)的治疗[2]。但国内应用该药后的临床数据较少,其安全性分析鲜有报道,本研究旨在探讨经我中心治疗的32位CD30+恶性淋巴瘤患者应用维布妥昔单抗的疗效及不良反应,为临床提供参考。
1 资料与方法
1.1 临床资料
收集2021年1月-2022年8月就诊于郑州大学第一附属医院接受维布妥昔单抗联合化疗治疗的32例恶性淋巴瘤患者病历资料。所有患者免疫组织化学结果均为CD30阳性。其中男17例、女15例。所有病例均接受含维布妥昔单抗的方案治疗至少2周期。中位年龄48岁(13~82岁)。该研究评估的终点包含从确诊至死亡或末次随访时间的总生存(OS)以及从确诊至疾病进展或末次随访时间的无进展生存(PFS)。本研究由郑州大学第一附属医院临床与研究伦理委员会批准,涉及人类参与者的所有程序均符合《赫尔辛基宣言》。
1.2 近期疗效评价及不良反应判定
每2个周期结束后采用CT或PET-CT等进行复查,依据Lugano标准[3]进行疗效评价,分为完全缓解(CR)、部分缓解(PR)、稳定(SD)以及进展(PD)。不良反应评价依照美国国立癌症研究所(NCI)关于通用不良事件术语标准(CT-CAE)5.0版分级标准,分为0~Ⅳ级。
1.3 治疗用量
维布妥昔单抗的使用按推荐剂量1.8 mg/kg,每三周一次(如果患者体重大于100 kg,则按照100 kg计算),30 min以上静脉输注给药。患者出现可耐受的不良反应时,亦可减量至1.2 mg/kg。也可按照1.2 mg/kg,每两周一次给药,儿童用药剂量与成人一致[4]。
1.4 统计学方法
SPSS26.0软件对检测数据进行统计学分析。生存分析采用Kaplan-Meier检验法,P < 0.05为差异有统计学意义。
2 结果
2.1 一般情况
32例接受BV治疗的淋巴瘤患者,包含霍奇金淋巴瘤14例、弥漫大B细胞淋巴瘤2例、成熟T/NK细胞淋巴瘤16例(含间变大细胞淋巴瘤10例、血管免疫母细胞性T细胞淋巴瘤3例、结外NK/T细胞淋巴瘤1例、外周T细胞淋巴瘤-非特指型2例)。均为一线化疗后无效或复发。其中男17例、女15例,男女比例为1.1:1。 < 60岁23例、≥60岁9例,中位年龄48岁。东部肿瘤协作组制定的评价体能活动状态(ECOG PS)评分≥2分者15例。用药时患有Ⅲ期和Ⅳ期疾病的患者30例(94%)。9例在维布妥昔治疗期间因经济原因而终止用药,基本临床特征见表 1。
表 1 32例恶性淋巴瘤患者的基本临床特征Table 1 Clinical features of 32 patients with malignant lymphoma
2.2 疗效
32例患者接受了至少2周期的维布妥昔单抗治疗,在2周期末进行疗效评估时,3例患者未入院,疗效未能评估。其余患者中2例CR,15例PR,总体缓解率(ORR)为53%,SD 8例,PD 4例。4周期末评估时,6例患者因经济原因、强烈的不良反应而停药,其余患者CR 7例、PR 9例,ORR为55%,SD 1例、PD 2例。9例患者继续治疗达到6周期以上,6周期末评估结果提示,CR 2例、PR 3例,PD 4例。1例患者使用维布妥昔单抗治疗达到8周期时获得CR。4周期治疗结束后,霍奇金淋巴瘤CR率略高于外周T细胞淋巴瘤(28.6% vs. 20.0%),但总体缓解率低于外周T细胞淋巴瘤(42.9% vs. 66.7%),见表 2。OS及PFS中位生存期均未达到,见图 1。
表 2 维布妥昔单抗应用4周期后各类淋巴瘤反应情况及不良反应(n(%))Table 2 Response and adverse events of various types of lymphoma after four cycles of brentuximab vedotin (n(%))
2.3 安全性
在14例霍奇金淋巴瘤患者中,6例发生了3级以上的不良反应,略低于外周T细胞淋巴瘤患者3级及以上不良反应发生率(42.9% vs.46.7%),见表 2。32位患者均发生不良反应,1~ 2级16例(50.0%),3级及以上16例(50.0%)。11例(34.3%)患者用药后发生1种不良反应、4例(12.5%)患者发生2种类型不良反应、10例(31.3%)患者发生3种类型不良反应、5例(15.6%)患者发生4种类型不良反应、2例(6.3%)患者发生5种类型不良反应。4例患者分别因发生过敏、重症肺炎、肝脏损伤导致的转氨酶增高以及麻痹性肠梗阻停止使用维布妥昔单抗。最常见的不良反应为任何级别的中性粒细胞减少(50%)和肺炎(46.9%),3级以上粒细胞缺乏症发生率并不高(6.3%),但3级及以上肺炎发生率为18.8%,并且有2例患者死于重症肺炎。贫血发生率虽高(43.8%),但大部分均为1、2级不良反应。发热性中性粒细胞减少症的发生率为25%,3级以上的发生率为12.5%。外周神经症状的患者占21.9%,但无3级不良反应,见表 3。非成人用药的不良事件和成人相似,主要集中在中性粒细胞减少(3/5),其他不良事件见表 4。
表 3 32例恶性淋巴瘤患者的不良反应发生情况Table 3 Adverse events in patients 表 4 非成人患者一般情况及不良反应Table 4 General condition and adverse events of juvenile patients
表 4 非成人患者一般情况及不良反应Table 4 General condition and adverse events of juvenile patients
3 讨论
CD30是肿瘤坏死因子受体(TNFR)超家族中的一员,又名TNFRSF8,是一种Ⅰ型跨膜糖蛋白受体。正常个体仅在部分免疫母细胞中表达CD30[5],选择性地表达于恶性淋巴细胞,其中最常见的有经典型霍奇金淋巴瘤和间变大细胞淋巴瘤。CD30配体CD30L(CD153又名TNFSF8)是一种兼具水溶性和脂溶性的Ⅱ型跨膜蛋白。二者结合后激活了NF-κB通路并使STAT3和STAT6磷酸化,从而加速细胞增殖、抑制其凋亡[6]。维布妥昔单抗作为一种新型ADC类药物,兼具精准靶向和高效杀瘤的效应,在临床方面的应用正在被逐渐探索。
一项Ⅱ期临床研究报道,单药维布妥昔单抗按照每三周一次1.8 mg/kg的剂量应用于复发性/难治性间变大细胞淋巴瘤患者,完全缓解率为57%,客观缓解率达86%,且BV单药治疗患者可获得持久缓解,中位持续响应时间(duration of response, DOR)为12.6个月[7]。另一项单药治疗复发性/难治性非霍奇金淋巴瘤(relapsed/refractory non-Hodgkin lymphoma, R/R NHL)的研究中,可评估的患者CR率为24%,ORR为41%[8]。维布妥昔单抗联合吉西他滨治疗复发性/难治性外周T细胞淋巴瘤患者的完全缓解率为19.7%,ORR为47.9%,显著高于吉西他滨单药应用[9]。在另一项维布妥昔单抗联合化疗治疗外周T细胞淋巴瘤的Ⅲ期临床试验中表明,维布妥昔联合CHP方案的疗效显著优于CHOP方案,且提高存活率的同时并没有观察到毒性的增加[10]。目前美国血液与骨髓移植协会(ASBMT)、国际血液和骨髓移植研究中心(CIBMTR)和欧洲骨髓移植协会(EBMT)淋巴瘤工作组均推荐BV联合化疗作为复发/难治霍奇金淋巴瘤自体造血干细胞移植(autologous hematopoietic stem cell transplantation, ASCT)之前的巩固治疗[11]。国外临床试验报道维布妥昔单抗联合吉西他滨治疗儿童难治性霍奇金淋巴瘤可将完全缓解率提高至67%,为患者快速进行高剂量化疗和自体干细胞拯救巩固提供机会[12]。在一项复发或难治性经典霍奇金淋巴瘤和系统性间变性大细胞淋巴瘤儿童患者的1/2期研究中,总体缓解率为46%,完全缓解率为34%,安全情况与在成人中报告的安全情况一致[4]。有研究表明,维布妥昔单抗联合化疗治疗初治儿童ALK阳性ALCL,2周期后完全缓解率可达62%,6周期后完全缓解率可达97%[13]。本研究包含5例12~18岁非成人患者,其中霍奇金淋巴瘤患者3例,外周细胞淋巴瘤2例。1例患者4周期后达到完全缓解;1例患者4周期后达到部分缓解,因经济原因而拒绝再次用药;1例患者2周期后达到部分缓解,因经济原因拒绝继续用药;2例患者2周期后疾病稳定,分别因4级过敏反应和3级白细胞减少而停止用药。中性粒细胞减少仍是非成人患者中最常见的不良事件。CSCO指南现已将维布妥昔纳入到复发难治性霍奇金淋巴瘤的二线治疗中,儿童ALCL目前尚缺乏标准治疗方案,但综上,维布妥昔联合化疗的治疗效果明确,不良反应可控,可纳入临床治疗的考虑范围。
本研究回顾性分析一组复发难治性恶性淋巴瘤患者,采用化疗联合维布妥昔单抗进行治疗。4周期治疗后患者CR率为22%,其中,霍奇金淋巴瘤CR率为28.6%,外周T细胞淋巴瘤为20.0%,霍奇金淋巴瘤患者总体缓解率为42.9%,低于外周T细胞淋巴瘤(66.7%)。3级及以上不良反应发生率为50.0%,这与Locatelli等研究结果相似[4]。另外,CD30阳性的弥漫大B细胞淋巴瘤患者及NK/T细胞淋巴瘤患者应用4周期后均疾病进展,且均发生3级及以上不良反应,但因本次研究纳入病例数过少,其疗效及安全性在CD30阳性的弥漫大B细胞淋巴瘤及NK/T细胞淋巴瘤需要更加深入探讨。目前,以BV为基础的治疗方案正在探索中,BV联合其他药物治疗有望进一步改善CD30+恶性淋巴瘤患者的临床现状,改善其预后。
Competing interests: The authors declare that they have no competing interests.作者贡献:张雪:文献查阅、论文撰写尹君丽、王稼祥:文献检索石文贵:论文修改焦作义:整体思路设计及论文指导 -
表 1 茶黄素类天然产物在癌症中的作用
Table 1 Role of theaflavins natural products in cancer

-
[1] Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries[J]. CA Cancer J Clin, 2021, 71(3): 209-249. doi: 10.3322/caac.21660
[2] Smyth EC, Nilsson M, Grabsch HI, et al. Gastric cancer[J]. Lancet, 2020, 396(10251): 635-648. doi: 10.1016/S0140-6736(20)31288-5
[3] Wu C, Li M, Meng H, et al. Analysis of status and countermeasures of cancer incidence and mortality in China[J]. Sci China Life Sci, 2019, 62(5): 640-647. doi: 10.1007/s11427-018-9461-5
[4] Luo T, Jiang JG. Anticancer Effects and Molecular Target of Theaflavins from Black Tea Fermentation in Vitro and in Vivo[J]. J Agric Food Chem, 2021, 69(50): 15052-15065. doi: 10.1021/acs.jafc.1c05313
[5] 刘昌伟, 张梓莹, 王俊懿, 等. 茶黄素生物学活性研究进展[J]. 食品科学, 2021. [网络首发] Liu CW, Zhang ZY, Wang JY, et al. Research Progress on bioactivity of theaflavins[J]. Shi Pin Ke Xue, 2021. [Online ahead of print]
[6] Takemoto M, Takemoto H. Synthesis of Theaflavins and Their Functions[J]. Molecules, 2018, 23(4): 918. doi: 10.3390/molecules23040918
[7] O'Neill EJ, Termini D, Albano A, et al. Anti-Cancer Properties of Theaflavins[J]. Molecules, 2021, 26(4): 987. doi: 10.3390/molecules26040987
[8] Pan H, Kim E, Rankin GO, et al. Theaflavin-3, 3'-Digallate Enhances the Inhibitory Effect of Cisplatin by Regulating the Copper Transporter 1 and Glutathione in Human Ovarian Cancer Cells[J]. Int J Mol Sci, 2018, 19(1): 117. doi: 10.3390/ijms19010117
[9] Pan H, Li J, Rankin GO, et al. Synergistic effect of black tea polyphenol, theaflavin-3, 3'-digallate with cisplatin against cisplatin resistant human ovarian cancer cells[J]. J Funct Foods, 2018, 46: 1-11. doi: 10.1016/j.jff.2018.04.037
[10] Liu Z, de Bruijn WJC, Bruins ME, et al. Microbial Metabolism of Theaflavin-3, 3'-digallate and Its Gut Microbiota Composition Modulatory Effects[J]. J Agric Food Chem, 2021, 69(1): 232-245. doi: 10.1021/acs.jafc.0c06622
[11] Chen T, Yang CS. Biological fates of tea polyphenols and their interactions with microbiota in the gastrointestinal tract: implications on health effects[J]. Crit Rev Food Sci Nutr, 2020, 60(16): 2691-2709. doi: 10.1080/10408398.2019.1654430
[12] Balaji S, Terrero D, Tiwari AK, et al. Alternative approaches to overcome chemoresistance to apoptosis in cancer[J]. Adv Protein Chem Struct Biol, 2021, 126: 91-122.
[13] Carneiro BA, El-Deiry WS. Targeting apoptosis in cancer therapy[J]. Nat Rev Clin Oncol, 2020, 17(7): 395-417. doi: 10.1038/s41571-020-0341-y
[14] Gao Y, Yin J, Tu Y, et al. Theaflavin-3, 3'-Digallate Suppresses Human Ovarian Carcinoma OVCAR-3 Cells by Regulating the Checkpoint Kinase 2 and p27 kip1 Pathways[J]. Molecules, 2019, 24(4): 673. doi: 10.3390/molecules24040673
[15] Tu Y, Kim E, Gao Y, et al. Theaflavin-3, 3'-digallate induces apoptosis and G2 cell cycle arrest through the Akt/MDM2/p53 pathway in cisplatin-resistant ovarian cancer A2780/CP70 cells[J]. Int J Oncol, 2016, 48(6): 2657-2665. doi: 10.3892/ijo.2016.3472
[16] Lahiry L, Saha B, Chakraborty J, et al. Theaflavins target Fas/caspase-8 and Akt/pBad pathways to induce apoptosis in p53-mutated human breast cancer cells[J]. Carcinogenesis, 2010, 31(2): 259-268. doi: 10.1093/carcin/bgp240
[17] Imran A, Butt MS, Xiao H, et al. Inhibitory effect of black tea (Camellia sinensis) theaflavins and thearubigins against HCT 116 colon cancer cells and HT 460 lung cancer cells[J]. J Food Biochem, 2019, 43(5): e12822. doi: 10.1111/jfbc.12822
[18] Xu XY, Zhao CN, Cao SY, et al. Effects and mechanisms of tea for the prevention and management of cancers: An updated review[J]. Crit Rev Food Sci Nutr, 2020, 60(10): 1693-1705. doi: 10.1080/10408398.2019.1588223
[19] Petroni G, Formenti SC, Chen-Kiang S, et al. Immunomodulation by anticancer cell cycle inhibitors[J]. Nat Rev Immunol, 2020, 20(11): 669-679. doi: 10.1038/s41577-020-0300-y
[20] Chakrabarty S, Das A, Bhattacharya A, et al. Theaflavins depolymerize microtubule network through tubulin binding and cause apoptosis of cervical carcinoma HeLa cells[J]. J Agric Food Chem, 2011, 59(5): 2040-2048. doi: 10.1021/jf104231b
[21] Chakrabarty S, Nag D, Ganguli A, et al. Theaflavin and epigallocatechin-3-gallate synergistically induce apoptosis through inhibition of PI3K/Akt signaling upon depolymerizing microtubules in HeLa cells[J]. J Cell Biochem, 2019, 120(4): 5987-6003. doi: 10.1002/jcb.27886
[22] Tan Q, Peng L, Huang Y, et al. Structure-Activity Relationship Analysis on Antioxidant and Anticancer Actions of Theaflavins on Human Colon Cancer Cells[J]. J Agric Food Chem, 2019, 67(1): 159-170. doi: 10.1021/acs.jafc.8b05369
[23] Ding Y, Chen B, Gao Z, et al. Pre-treated theaflavin-3, 3'-digallate has a higher inhibitory effect on the HCT116 cell line[J]. Food Nutr Res, 2017, 61(1): 1400340. doi: 10.1080/16546628.2017.1400340
[24] Shi W, Zhang G, Ma Z, et al. Hyperactivation of HER2-SHCBP1-PLK1 axis promotes tumor cell mitosis and impairs trastuzumab sensitivity to gastric cancer[J]. Nat Commun, 2021, 12(1): 2812. doi: 10.1038/s41467-021-23053-8
[25] Zhang Y, Zhang Z. The history and advances in cancer immunotherapy: understanding the characteristics of tumor-infiltrating immune cells and their therapeutic implications[J]. Cell Mol Immunol, 2020, 17(8): 807-821. doi: 10.1038/s41423-020-0488-6
[26] Chattopadhyay S, Bhattacharyya S, Saha B, et al. Tumor-shed PGE(2) impairs IL2Rgammac-signaling to inhibit CD4 T cell survival: regulation by theaflavins[J]. PLoS One, 2009, 4(10): e7382. doi: 10.1371/journal.pone.0007382
[27] Lee S, Rauch J, Kolch W. Targeting MAPK Signaling in Cancer: Mechanisms of Drug Resistance and Sensitivity[J]. Int J Mol Sci, 2020, 21(3): 1102. doi: 10.3390/ijms21031102
[28] Pan H, Wang F, Rankin GO, et al. Inhibitory effect of black tea pigments, theaflavin-3/3'-gallate against cisplatin-resistant ovarian cancer cells by inducing apoptosis and G1 cell cycle arrest[J]. Int J Oncol, 2017, 51(5): 1508-1520. doi: 10.3892/ijo.2017.4145
[29] Gao Y, Li W, Jia L, et al. Enhancement of (-)-epigallocatechin-3-gallate and theaflavin-3-3'-digallate induced apoptosis by ascorbic acid in human lung adenocarcinoma SPC-A-1 cells and esophageal carcinoma Eca-109 cells via MAPK pathways[J]. Biochem Biophys Res Commun, 2013, 438(2): 370-374. doi: 10.1016/j.bbrc.2013.07.078
[30] Zhang L, Meng S, Yan B, et al. Anti-Proliferative, Pro-Apoptotic, Anti-Migrative and Tumor-Inhibitory Effects and Pleiotropic Mechanism of Theaflavin on B16F10 Melanoma Cells[J]. Onco Targets Ther, 2021, 14: 1291-1304. doi: 10.2147/OTT.S286350
[31] Zhang L, Yan B, Meng S, et al. Theaflavin Induces Apoptosis of A375 Human Melanoma Cells and Inhibits Tumor Growth in Xenograft Zebrafishes Through P53- and JNK-Related Mechanism[J]. Front Pharmacol, 2020, 11: 1317. doi: 10.3389/fphar.2020.01317
[32] Tewari D, Patni P, Bishayee A, et al. Natural products targeting the PI3K-Akt-mTOR signaling pathway in cancer: A novel therapeutic strategy[J]. Semin Cancer Biol, 2022, 80: 1-17. doi: 10.1016/j.semcancer.2019.12.008
[33] Halder B, Das Gupta S, Gomes A. Black tea polyphenols induce human leukemic cell cycle arrest by inhibiting Akt signaling: possible involvement of Hsp90, Wnt/β-catenin signaling and FOXO1[J]. FEBS J, 2012, 279(16): 2876-2891. doi: 10.1111/j.1742-4658.2012.08668.x
[34] Mazumdar M, Adhikary A, Chakraborty S, et al. Targeting RET to induce medullary thyroid cancer cell apoptosis: an antagonistic interplay between PI3K/Akt and p38MAPK/caspase-8 pathways[J]. Apoptosis, 2013, 18(5): 589-604. doi: 10.1007/s10495-013-0803-0
[35] Doheny D, Manore SG, Wong GL, et al. Hedgehog Signaling and Truncated GLI1 in Cancer[J]. Cells, 2020, 9(9): 2114. doi: 10.3390/cells9092114
[36] Sur S, Pal D, Mandal S, et al. Tea polyphenols epigallocatechin gallete and theaflavin restrict mouse liver carcinogenesis through modulation of self-renewal Wnt and hedgehog pathways[J]. J Nutr Biochem, 2016, 27: 32-42. doi: 10.1016/j.jnutbio.2015.08.016
[37] Sur S, Pal D, Roy R, et al. Tea polyphenols EGCG and TF restrict tongue and liver carcinogenesis simultaneously induced by N-nitrosodiethylamine in mice[J]. Toxicol Appl Pharmacol, 2016, 300: 34-46. doi: 10.1016/j.taap.2016.03.016
[38] Khan H, Ullah H, Castilho PCMF, et al. Targeting NF-κB signaling pathway in cancer by dietary polyphenols[J]. Crit Rev Food Sci Nutr, 2020, 60(16): 2790-2800. doi: 10.1080/10408398.2019.1661827
[39] Adhikary A, Mohanty S, Lahiry L, et al. Theaflavins retard human breast cancer cell migration by inhibiting NF-kappaB via p53-ROS cross-talk[J]. FEBS Lett, 2010, 584(1): 7-14. doi: 10.1016/j.febslet.2009.10.081
[40] Singh M, Singh R, Bhui K, et al. Tea polyphenols induce apoptosis through mitochondrial pathway and by inhibiting nuclear factor-kappaB and Akt activation in human cervical cancer cells[J]. Oncol Res, 2011, 19(6): 245-257. doi: 10.3727/096504011X13021877989711
[41] Xin P, Xu X, Deng C, et al. The role of JAK/STAT signaling pathway and its inhibitors in diseases[J]. Int Immunopharmacol, 2020, 80: 106210. doi: 10.1016/j.intimp.2020.106210
[42] Liu W, Li J. Theaflavin-3, 3'-Digallate Attenuates Rheumatoid Inflammation in Mice Through the Nuclear Factor-κB and MAPK Pathways[J]. Arch Immunol Ther Exp (Warsz), 2019, 67(3): 153-160. doi: 10.1007/s00005-019-00536-7
[43] Mandal D, Bhattacharyya S, Lahiry L, et al. Black tea-induced decrease in IL-10 and TGF-beta of tumor cells promotes Th1/Tc1 response in tumor bearer[J]. Nutr Cancer, 2007, 58(2): 213-221. doi: 10.1080/01635580701328503
[44] Bhattacharyya A, Mandal D, Lahiry L, et al. Black tea protects immunocytes from tumor-induced apoptosis by changing Bcl-2/Bax ratio[J]. Cancer Lett, 2004, 209(2): 147-154. doi: 10.1016/j.canlet.2003.12.025
[45] Mandal D, Lahiry L, Bhattacharyya A, et al. Tumor-induced thymic involution via inhibition of IL-7R alpha and its JAK-STAT signaling pathway: protection by black tea[J]. Int Immunopharmacol, 2006, 6(3): 433-444. doi: 10.1016/j.intimp.2005.09.005
[46] Zhang Y, Wang X. Targeting the Wnt/β-catenin signaling pathway in cancer[J]. J Hematol Oncol, 2020, 13(1): 165. doi: 10.1186/s13045-020-00990-3
[47] Sferrazza G, Corti M, Brusotti G, et al. Nature-derived compounds modulating Wnt/ β -catenin pathway: a preventive and therapeutic opportunity in neoplastic diseases[J]. Acta Pharm Sin B, 2020, 10(10): 1814-1834. doi: 10.1016/j.apsb.2019.12.019
[48] Pan H, Kim E, Rankin GO, et al. Theaflavin-3, 3'-digallate inhibits ovarian cancer stem cells via suppressing Wnt/β-Catenin signaling pathway[J]. J Funct Foods, 2018, 50: 1-7. doi: 10.1016/j.jff.2018.09.021
[49] Gao Y, Rankin GO, Tu Y, et al. Theaflavin-3, 3'-digallate decreases human ovarian carcinoma OVCAR-3 cell-induced angiogenesis via Akt and Notch-1 pathways, not via MAPK pathways[J]. Int J Oncol, 2016, 48(1): 281-292. doi: 10.3892/ijo.2015.3257
[50] Bhattacharya R, Chatterjee R, Mandal AKA, et al. Theaflavin-Containing Black Tea Extract: A Potential DNA Methyltransferase Inhibitor in Human Colon Cancer Cells and Ehrlich Ascites Carcinoma-Induced Solid Tumors in Mice[J]. Nutr Cancer, 2021: 73(11-12): 2447-2459. doi: 10.1080/01635581.2020.1828943



 下载:
下载: