Cordycepin Attenuates Immune Function Injury in A Rat Model of Lung Cancer After Radiotherapy by Inhibiting JAK2/STAT3 Pathway
-
摘要:目的
探讨虫草素通过JAK2/STAT3信号通路对肺癌大鼠放射性治疗免疫功能损伤的抑制作用。
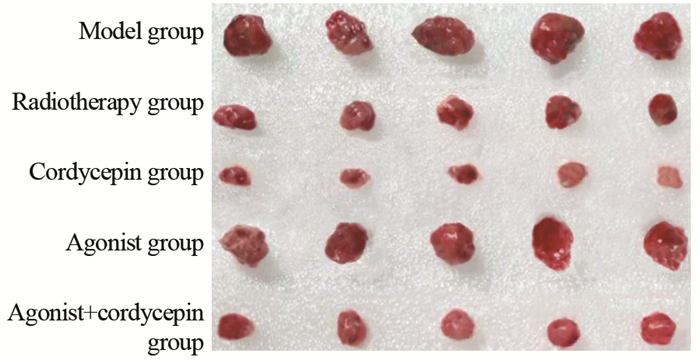
方法50只大鼠建立荷瘤模型,另设正常组(10只)。建模成功大鼠随机分为模型组、放疗组、虫草素组、激动剂组和激动剂+虫草素组,每组10只。比较各组大鼠瘤重、肿瘤体积、抑瘤率、IL-6、TNF-α、脾指数、胸腺指数、T淋巴细胞亚群数量、JAK2、p-JAK2、STAT3和p-STAT3蛋白表达水平。
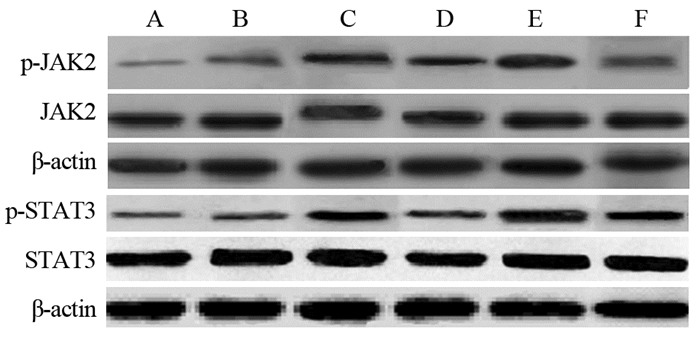
结果与正常组比较,模型组IL-6、TNF-α、CD8+、p-JAK2、p-STAT3升高,脾指数、胸腺指数、CD4+、CD4+/CD8+降低(P < 0.05);与模型组比较,放疗组瘤重、肿瘤体积、脾指数、胸腺指数、CD4+、CD4+/CD8+降低,IL-6、TNF-α、CD8+、p-JAK2和p-STAT3升高(P < 0.05);与放疗组比较,虫草素组瘤重、肿瘤体积、IL-6、TNF-α、CD8+、p-JAK2、p-STAT3降低,抑瘤率、脾指数、胸腺指数、CD4+、CD4+/CD8+升高,激动剂组瘤重、肿瘤体积、IL-6、TNF-α、CD8+、p-JAK2、p-STAT3升高,抑瘤率、脾指数、胸腺指数、CD4+、CD4+/CD8+降低(P < 0.05);与激动剂+虫草素组比较,虫草素组瘤重、肿瘤体积、IL-6、TNF-α、CD8+、p-JAK2、p-STAT3降低,抑瘤率、脾指数、胸腺指数、CD4+、CD4+/CD8+升高,激动剂组瘤重、肿瘤体积、IL-6、TNF-α、CD8+、p-JAK2、p-STAT3升高,抑瘤率、脾指数、胸腺指数、CD4+、CD4+/CD8+降低(P < 0.05)。
结论虫草素可有效抑制肺癌大鼠放射性治疗免疫功能损伤,其机制可能通过抑制JAK2/STAT3信号通路蛋白表达发挥调控作用。
-
关键词:
- 虫草素 /
- 放疗 /
- 免疫功能 /
- JAK2/STAT3
Abstract:ObjectiveTo investigate the inhibitory effect of cordycepin on immune function injury in lung cancer rats after radiation therapy through JAK2/STAT3 signaling pathway.
MethodsFifty rats were used to establish tumor-bearing model and other 10 rats were taken as normal group. After successful modeling, the rats were randomly divided into model group, radiotherapy group, cordycepin group, agonist group and agonist+cordycepin group (10 rats in each group). We compared tumor weight, tumor volume, tumor inhibition rate, IL-6, TNF-α, spleen index and thymus index, the number of T lymphocyte subsets, JAK2, p-JAK2, STAT3 and p-STAT3 protein expression levels among all groups.
ResultsCompared with normal group, IL-6, TNF-α, CD8+, p-JAK2 and p-STAT3 in model group were increased, while spleen index, thymus index, CD4+ and CD4+/CD8+ were decreased (P < 0.05). Compared with model group, tumor weight, tumor volume, spleen index, thymus index, CD4+ and CD4+/CD8+ were decreased in radiotherapy group, while IL-6, TNF-α, CD8+, p-JAK2 and p-STAT3 were increased (P < 0.05). Compared with radiotherapy group, tumor weight, tumor volume, IL-6, TNF-α, CD8+, p-JAK2 and p-STAT3 were decreased in cordycepin group, while tumor inhibition rate, spleen index thymus index, CD4+ and CD4+/CD8+ were increased; tumor weight, tumor volume, IL-6, TNF-α, CD8+, p-JAK2 and p-STAT3 protein expression were increased in agonist group, while tumor inhibition rate, spleen index, thymus index, CD4+ and CD4+/CD8+ were decreased (P < 0.05). Compared with agonist+cordycepin group, tumor weight, tumor volume, IL-6, TNF-α, CD8+, p-JAK2 and p-STAT3 were decreased in cordycepin group, while tumor inhibition rate, spleen index, thymus index, CD4+ and CD4+/CD8+ were increased; tumor weight, tumor volume, IL-6, TNF-α, CD8+, p-JAK2 and p-STAT3 were increased in agonist group, while tumor inhibition rate, spleen index, thymus index, CD4+ and CD4+/CD8+ were decreased (P < 0.05).
ConclusionCordycepin can effectively inhibit the immune function injury in lung cancer rats after radiation therapy, and may play a regulatory role by inhibiting the JAK2/STAT3 signal pathway.
-
Key words:
- Cordycepin /
- Radiation therapy /
- Immune function /
- JAK2/STAT3
-
Competing interests: The authors declare that they have no competing interests.作者贡献:刘建波:实验设计及论文撰写李白羽:实验实施和资料收集柯善保:论文撰写张伟:论文修订和审校
-
表 1 各组大鼠瘤重、肿瘤体积和抑瘤率比较(x±s)
Table 1 Comparison of tumor weight, tumor volume and tumor inhibition rate of rats among five groups (x±s)

表 2 各组大鼠血清IL-6和TNF-α水平比较(x±s)
Table 2 Comparison of IL-6 and TNF-α levels in serum of rats among all groups (x±s)

表 3 各组大鼠脾指数和胸腺指数比较(x±s)
Table 3 Comparison of spleen index and thymus index among all groups (x±s)

表 4 各组大鼠脾脏T淋巴细胞亚群数量比较(x±s)
Table 4 Comparison of T lymphocyte subsets number in spleen of rats among all groups (x±s)

表 5 脾脏组织中JAK2、p-JAK2、STAT3和p-STAT3蛋白表达(x±s)
Table 5 Comparison of JAK2, p-JAK2, STAT3 and p-STAT3 protein levels in spleen of rats among all groups (x±s)

-
[1] 宋春洋, 祝淑钗, 沈文斌, 等. 临床Ⅲ期食管癌患者放疗前后免疫功能及外周血炎症指标对预后的影响分析[J]. 中华放射医学与防护杂志, 2020, 40(3): 189-195. doi: 10.3760/cma.j.issn.0254-5098.2020.03.006 Song CY, Zhu SC, Shen WB, et al. Analysis of the effects of immunity index and blood inflammatory markers pre- and post-radiotherapy on prognosis of clinical stage Ⅲ esophageal cancer patients[J]. Zhonghua Fang She Yi Xue Yu Fang Hu Za Zhi, 2020, 40(3): 189-195. doi: 10.3760/cma.j.issn.0254-5098.2020.03.006
[2] 王多, 鲍荣, 王芳, 等. 虫草素抗肿瘤作用分子机制研究进展[J]. 中国药理学与毒理学杂志, 2015, 29(4): 643-650. doi: 10.3867/j.issn.1000-3002.2015.04.018 Wang D, Bao R, Wang F, et al. progress in molecular mechanisms of anticancer action of corycepin[J]. Zhongguo Yao Li Xue Yu Du Li Xue Za Zhi, 2015, 29(4): 643-650. doi: 10.3867/j.issn.1000-3002.2015.04.018
[3] Zhang Y, Zhang XX, Yuan RY, et al. Cordycepin induces apoptosis in human pancreatic cancer cells via the mitochondrial-mediated intrinsic pathway and suppresses tumor growth in vivo[J]. Onco Targets Ther, 2018, 11: 4479-4490. doi: 10.2147/OTT.S164670
[4] Wang C, Mao ZP, Wang L, et al. Cordycepin inhibits cell growth and induces apoptosis in human cholangiocarcinoma[J]. Neoplasma, 2017, 64(6): 834-839. doi: 10.4149/neo_2017_604
[5] Lin YT, Liang SM, Wu YJ, et al. Cordycepin suppresses endothelial cell proliferation, migration, angiogenesis, and tumor growth by regulating focal adhesion kinase and p53[J]. Cancers(Basel), 2019, 11(2): 168. http://www.onacademic.com/detail/journal_1000041694748599_3052.html
[6] 韩丹, 崔琳琳, 王莹, 等. 虫草素药理作用研究进展[J]. 食品工业科技, 2019, 40(9): 335-338, 345. https://www.cnki.com.cn/Article/CJFDTOTAL-SPKJ201909057.htm Han D, Cui LL, Wang Y, et al. Research Progress On Pharmacological Effects Of Cordycepin[J]. Shi Pin Gong Ye Ke Ji, 2019, 40(9): 335-338, 345. https://www.cnki.com.cn/Article/CJFDTOTAL-SPKJ201909057.htm
[7] Mao Y, Yang D, He J, et al. Epidemiology of lung cancer[J]. Surg Oncol Clin N Am, 2016, 25(3): 439-445. doi: 10.1016/j.soc.2016.02.001
[8] Michaelidesová A, Konířová J, Bartůněk P, et al. Effects of radiation therapy on neural stem cells[J]. Genes(Basel), 2019, 10(9): 640. http://www.ncbi.nlm.nih.gov/pubmed/31450566
[9] Kirova Y, Tallet A, Aznar MC, et al. Radio-induced cardiotoxicity: from physiopathology and risk factors to adaptation of radiotherapy treatment planning and recommended cardiac follow-up[J]. Cancer Radiother, 2020, 24(6-7): 576-585. doi: 10.1016/j.canrad.2020.07.001
[10] Weichselbaum RR, Liang H, Deng L, et al. Radiotherapy and immunotherapy: a beneficial liaison?[J]. Nat Rev Clin Oncol, 2017, 14(6): 365-379. doi: 10.1038/nrclinonc.2016.211
[11] Woolley VC, Teakle GR, Prince G, et al. Cordycepin, a metabolite of Cordyceps militaris, reduces immune-related gene expression in insects[J]. J Invertebr Pathol, 2020, 177: 107480. doi: 10.1016/j.jip.2020.107480
[12] Lei J, Wei Y, Song P, et al. Cordycepin inhibits LPS-induced acute lung injury by inhibiting inflammation and oxidative stress[J]. Eur J Pharmacol, 2018, 818: 110-114. doi: 10.1016/j.ejphar.2017.10.029
[13] Tan L, Song X, Ren Y, et al. Anti-inflammatory effects of cordycepin: A review[J]. Phytother Res, 2020. Online ahead of print.
[14] 安青, 何立巍, 吴红雁, 等. 虫草素通过调节CD4+T淋巴细胞PD-1受体促进肿瘤免疫及机制研究[J]. 南京中医药大学学报, 2018, 34(5): 495-498. https://www.cnki.com.cn/Article/CJFDTOTAL-NJZY201805015.htm An Q, He LW, Wu HY, et al. Mechanism of cordycepin promotes tumor immunity by regulating PD-1 receptor of CD4+T lymphocytes[J]. Nanjing Zhong Yi Yao Da Xue Xue Bao, 2018, 34(5): 495-498. https://www.cnki.com.cn/Article/CJFDTOTAL-NJZY201805015.htm
[15] Zundler S, Neurath MF. Integrating immunologic signaling networks: the JAK/STAT pathway in colitis and colitis-associated cancer[J]. Vaccines(Basel), 2016, 4(1): 5. http://www.onacademic.com/detail/journal_1000040540984510_5b25.html
[16] Yu T, Li Z, Xu L, et al. Anti-inflammation effect of Qingchang suppository in ulcerative colitis through JAK2/STAT3 signaling pathway in vitro and in vivo[J]. J Ethnopharmacol, 2021, 266: 113442. doi: 10.1016/j.jep.2020.113442
[17] Qing Y, Stark GR. Alternative activation of STAT1 and STAT3 in response to interferon-gamma[J]. J Biol Chem, 2004, 279(40): 41679-41685. doi: 10.1074/jbc.M406413200
[18] Lei RE, Shi C, Zhang PL, et al. IL-9 promotes proliferation and metastasis of hepatocellular cancer cells by activating JAK2/STAT3 pathway[J]. Int J Clin Exp Pathol, 2017, 10(7): 7940-7946. http://www.researchgate.net/publication/326058664_IL-9_promotes_proliferation_and_metastasis_of_hepatocellular_cancer_cells_by_activating_JAK2STAT3_pathway
[19] Chen J, Zhang W, Xu Q, et al. Ang-(1-7) protects HUVECs from high glucose-induced injury and inflammation via inhibition of the JAK2/STAT3 pathway[J]. Int J Mol Med, 2018, 41(5): 2865-2878. http://www.spandidos-publications.com/ijmm/41/5/2865/download



 下载:
下载: