Establishment and Innovation of Malnutrition Diagnosis and Treatment System for Patients with Cancer in China
-
摘要:
肿瘤患者是营养不良的高危人群。营养不良是肿瘤患者最常见的合并症,是肿瘤患者独立的死亡风险因素。本文阐述了我国肿瘤患者营养不良诊断体系、治疗体系的建立和构架以及诊疗体系从初步认识到逐步建立并不断创新发展的历程。简述了目前临床普遍应用的肿瘤营养筛查及评估方法并对近些年临床应用中的新方法进行介绍,旨在为进一步优化该诊疗体系提供参考依据,助力提升我国肿瘤营养不良诊疗水平,改善患者预后,节约医疗费用。
Abstract:Patients with cancer are at high risk of malnutrition, which is the most common complication and independent risk factor for death in cancer patients. This article elaborates on the creation and structure of the diagnostic and treatment systems for cancer malnutrition in China, as well as the process from the initial understanding to the gradual establishment and continuous innovative development of the these systems. It briefly describes the commonly used methods for cancer nutrition screening and assessment in clinical practice at present and introduces the new methods in clinical application in recent years. The aim is to provide reference basis for further optimizing this diagnostic and treatment system, thereby improving the diagnosis and treatment level of cancer malnutrition in China, thus, enhancing the prognosis of patients and reducing the medical expenses.
-
Key words:
- Cancer /
- Malnutrition /
- Nutrition screening /
- Nutrition assessment /
- Nutrition treatment
-
0 引言
我国肿瘤的发病率呈逐年上升趋势,严重威胁国民身心健康、经济发展及社会稳定。肿瘤患者是营养不良的高危人群。研究表明,我国三级甲等医院住院肿瘤患者中,营养不良的发病率高达80%(轻度、中度及重度营养不良分别为22%、32%及26%)[1]。营养不良严重降低抗肿瘤治疗的疗效、增加治疗不良反应、降低患者生活质量、增加医疗费用。规范的营养治疗有改善肿瘤患者临床结局、提高生活质量以及节约医疗费用等重要作用。
营养不良是肿瘤患者最常见的合并症之一,直接导致30%~40%的肿瘤患者死亡[2]。营养是所有疾病康复的基础,也是患者自愈力和抗损伤的基石,营养治疗应该被作为一线治疗。近些年随着我国对重大慢病防控的关注与推进,针对肿瘤患者群体的规范化肿瘤营养诊断体系(包括营养筛查、营养评估、综合评价)及肿瘤营养治疗体系逐渐建立并完善。针对我国国民身体素质和营养状况研发了大量的营养筛查、营养评估工具,并对国外原有的营养诊断工具进行了创新与改良,协助临床医务人员更精准、快速的对患者营养状况进行评估,促进了临床营养的发展及肿瘤治疗的进步。
1 系统性构建肿瘤营养诊疗体系
1.1 营养不良的三级诊断
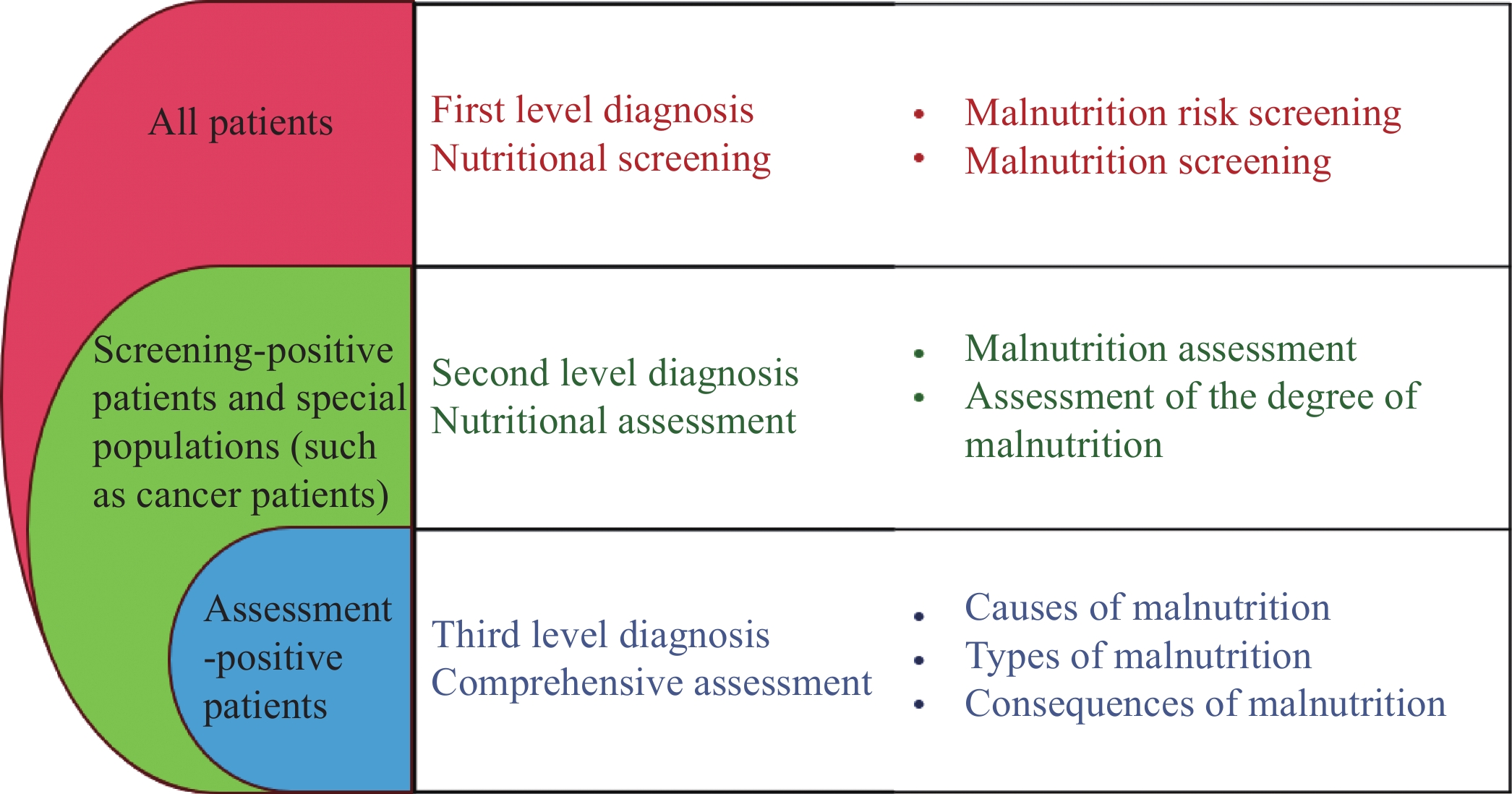
准确的营养不良诊断是制订营养治疗方案的基础。营养不良是一种全身性疾病,严重营养不良几乎影响所有器官和系统,甚至心理、精神及社会角色。肿瘤患者营养不良显著区别于良性疾病营养不良的特征,例如代谢水平升高、心理/生理应激、慢性炎性反应、代谢紊乱、骨骼肌丢失等,因而更加需要第三级别诊断。营养不良三级诊断体系是目前通用、公认的营养不良诊断标准,是肿瘤患者营养治疗的基石。传统的营养不良诊断流程只包括营养筛查和营养评估两个阶段[3]。由于肿瘤营养不良会导致更严重的炎性反应应激、代谢紊乱、肌肉减少、功能障碍,二级营养诊断(营养筛查+营养评估)难以充分了解营养不良对肿瘤患者的影响和全部严重后果[4]。2015年肿瘤患者营养不良三级诊断体系正式提出(见图1):营养筛查+营养评估+综合评价,即在二级诊断之后,对患者进行综合评价,综合评价涵盖了多维度与营养相关的内容,包括患者病史询问、器械检查、体格和体能检查、能耗水平、应激程度、代谢改变、免疫功能、心理及精神状况、器官功能等方面,分析营养不良的原因、类型及后果,了解营养不良对机体的影响,明确是否需要综合治疗和(或)制订治疗方案,三级诊断可以在确定患者营养不良程度的基础上,了解营养不良的原因及类型和可能产生的临床后果[5],从而决定是否对患者接下来进行营养治疗、炎性反应治疗、代谢调节治疗、免疫调节治疗、心理支持治疗和身体功能维护等相关措施。对于综合评价异常的患者,要对其实施综合治疗,包括营养教育、医学营养、炎性反应抑制、代谢调节治疗和免疫营养等。第三阶段诊断旨在借助营养护理来改善患者的整体健康状况[6]。
研究表明,肿瘤患者和手术患者中出现心理问题以及生活质量下降的比率尤其高[7]。饮食情况与生活质量和精神状况呈正相关。指南指出,肿瘤患者在入院后24小时内需启动三级营养诊断工作[8]。营养不良三级诊断是一个由浅入深的连续过程,由简单到复杂的发展过程,是一个集成创新的营养不良诊断方法。目前三级诊断体系已广泛应用于我国临床肿瘤治疗工作中,通过多年临床实践已经被证实是一种规范而实用的程序化方案。
1.2 营养不良五阶梯治疗
临床营养治疗存在治疗不足与治疗过度并存的情况,且营养治疗具有较大的随意性和差异性。2015年石汉平教授团队提出了营养不良五阶梯治疗体系的建立,五阶梯治疗原则提倡在对患者进行营养治疗时应首选营养教育(第一阶梯),然后依次沿阶梯向上晋级选择第二阶梯口服营养补充(Oral nutritional supplement, ONS)、第三阶梯全肠内营养(Total enteral nutrition, TEN)、第四阶梯部分肠外营养(Partial parenteral nutrition, PPN)联合部分肠内营养(Partial enteral nutrition, PEN)、第五阶梯全肠外营养(Total parenteral nutrition, TPN)[9]。五阶梯营养治疗原则明确指出,营养治疗应遵循膳食优先、口服优先、营养教育优先、肠内营养优先的四个优先原则[10]。高度重视营养教育,倡导口服营养补充,严格掌握肠外营养适应证。有效的纠正了临床营养治疗中营养不足和营养过度的双重问题,以及肠外营养、肠内营养使用比例倒置的问题,使临床营养治疗行为更加规范、合理,同时也降低了营养治疗相关费用。营养不良五阶梯治疗为临床提供了系统的营养不良治疗方法,通过不同阶梯的选择和应用,可满足不同患者的营养需求,具有经济实用、符合患者个性化治疗并能够全面满足营养需求等优势,在实际应用中,应根据患者的具体情况进行个体化治疗,以提高治疗效果,改善患者的生活质量和预后。实践表明,五阶梯治疗对肿瘤患者、肝硬化患者、老年多种疾病住院患者、新型冠状病毒肺炎等患者的治疗和康复起到重要作用[11-13]。
1.3 全程营养治疗理论
肿瘤患者的营养问题往往伴随其整个生命过程。全程营养治疗的定义是将营养治疗从医院内延伸到院外,系统构建分级、延续、全程的营养治疗,将治疗时间前移、疗程延长、空间拓展和外延扩大。
医院-社区(卫生服务机构)-家庭营养管理模式(Hospital-community health service organization-home, H-C-H)是针对肿瘤患者进行分级营养管理、三级联动、双向流通的营养管理模式[14]。将营养管理的范围由医院延伸到了社区和家庭,将营养管理的实施者由临床工作者扩展到患者家属、社区机构工作者和患者本人。将营养管理的目的由单纯的治疗疾病,扩展为提高患者生活质量、预防疾病、强身健体,从而将营养管理成为患者的终身管理。建立肿瘤整合康复营养体系,有利于我国肿瘤慢病化趋势下肿瘤患者全程营养治疗的规范应用[15]。规范化营养干预可以显著提高社区恶性肿瘤患者的营养状态和生活质量,从而改善预后[16-20]。患者在医院的治疗时间相较于患者生存期而言是短暂的,在院期间合理有效的营养支持可以改善患者治疗期间的营养状况,而漫长的居家营养管理则是提高患者生活质量、延长生存期、降低再入院率和并发症的重要因素[21-22],因此全程营养治疗理念具有重要意义。
2 营养筛查与评估技术
合理营养支持的前提是及时、准确的营养筛查与营养评估,明确的营养不良诊断是制订营养治疗方案的基础。文献报道的营养筛查量表有三十多种,目前国内外常规营养评估工具有全球营养不良领导倡议(the Global Leadership Initiative on Malnutrition, GLIM)、欧洲肠外肠内营养学会2015年营养不良专家共识(ESPEN 2015)、患者主观整体评估(the Patient-Generated Subjective Global Assessment, PG-SGA)、迷你营养评估量表(the Mini Nutritional Assessment, MNA)、营养风险筛查2002(Nutritional Risk Screening 2002, NRS2002)、营养不良通用筛查工具(Malnutrition Universal Screening Tool, MUST)、营养不良筛查工具(Malnutrition Screening Tool, MST)等[23-25]。不同的营养不良诊断工具各有其局限性,普适性较低,比如MNA更适用于老年患者。近年来国内在创新肿瘤营养诊疗关键技术方面取得重要突破,集成创新肿瘤营养诊疗关键技术大幅提高营养诊断效能。
2.1 发明营养筛查工具
2.1.1 肿瘤患者营养筛查工具(AIWW)
临床工作中需要容易理解、操作简便的营养筛查量表,AIWW基于德尔菲法将现有的25种营养筛查工具,总结了七个类型共25个条目的问题。通过两轮专家咨询针对中国肿瘤人群设计制作,最终确定了从年龄(A,Age)、摄入(I,Intake)、非自主体重丢失情况(W,Weight)、步行情况(W,Walk)4个方面进行筛查,为肿瘤患者的营养诊断提供了新的筛查工具[26],见表1。该量表显著提高营养筛查效率。通过数据库验证分析,以PG-SGA为金标准,将AIWW量表与现有医院常用营养不良筛查工具NRS2002以及MST进行营养不良筛查。研究显示AIWW具有比NS2002和MST更高的敏感度,并且AIWW具有不劣于NRS2002的临床获益率。
表 1 营养筛查工具AIWW问卷Table 1 AIWW screening questionnaireQuestions Yes No Q1: Age (A)—Are you over 65 years old? □ □ Q2: Intake (I)—Have you noticed a decrease in appetite or food intake in the past month? □ □ Q3: Weight (W)—Did you lose your weight involuntarily over the past month? □ □ Q4: Walking (W)—Did your walking pace, walking steps, or walking distance decrease
involuntarily over the past month?□ □ Notes: Yes (add 1 point) or No (0 points). A score of 1 or more=patient is at risk of malnutrition. 基于GLIM营养不良评估标准的实际应用中,AIWW是三种筛查工具中筛查能力与实际营养不良评估结合最好的筛查工具。作为营养筛查工具,更高的敏感度是其必备的条件。数据显示,AIWW漏诊率仅为0.9%,比国际目前最佳营养筛查工具NRS 2002的误诊率减少48.1%。提示AIWW是更适合肿瘤人群的营养筛查工具。AIWW设计极其简单,使用者不需要任何专业知识,四个条目可以由患者自身进行监测,如果得分提示营养不良高风险,早期及时给与患者营养支持治疗以获得更好的生活质量以及肿瘤治疗效果。同时,AIWW设计于实体肿瘤人群,所有肿瘤人群均可使用此工具进行监测。AIWW已经在肿瘤人群中获得了极为优秀的筛查效果,期待进一步在其他人群中对其有效性与敏感性进行验证与研究。
2.1.2 特异性营养评估工具
乳腺癌是全球范围内女性最常见的恶性肿瘤,对女性的健康和生命构成了严重的威胁[27]。预后营养指数(Prognostic nutritional index, PNI)是评估患者营养状况和预后的指标,包括血清白蛋白水平和淋巴细胞计数两种指数[28-29]。营养不良与乳腺癌患者的总体生存率下降相关,但对于乳腺癌患者预后最具预测性的营养指标尚未完全确定。常见的营养评估方法例如PG-SGA、GLIM、NRI和PNI对乳腺癌患者的特异性及敏感性均不理想,无法准确地评估患者营养状况及预后情况。
特异性营养评估工具(Cholesterol-modified prognostic nutritional index, CPNI)是在PNI的基础上添加总胆固醇作为矫正因子,是乳腺癌患者特异性营养评估工具。CPNI=4.8×胆固醇(mmol/L)− 1.5×白蛋白(g/L)− 7.7×白细胞(109/L)+ 126。CPNI进一步优化了PNI,在不同阶段的乳腺癌患者中都显示出优良的预测效果,是预测乳腺癌患者预后的极佳营养指标,并成功实现了良好的预后分层,预后预测效率比现有最佳工具提高12%[30]。为开发肿瘤患者营养评估工具提供了新思路。
2.1.3 炎症负荷指数
炎症负荷指数(Inflammatory burden index, IBI)是评估肿瘤患者炎症负荷的工具,即C反应蛋白、中性粒细胞和淋巴细胞的组合(IBI=C反应蛋白×中性粒细胞-淋巴细胞比值),并证实其是肿瘤患者强有力的预后预测指标[31]。大量研究显示,炎症负荷与肿瘤患者的预后密切相关,且不同的肿瘤类型其炎症负荷水平高低不同[32]。IBI可将肿瘤分为高、中、低炎症负荷三种类型,有效反映出肿瘤的代谢紊乱。与目前现有的系统性炎症生物标志物相比,IBI实现了良好的预后分层,是预测肿瘤预后最佳的生物标志物,为创新肿瘤治疗提供了重要思路[33-35]。
2.2 优化营养评估量表
GLIM标准以及PG-SGA都在肿瘤患者中进行了大量的验证,并且作为营养诊断方案被充分肯定其应用价值[36-39]。在临床实践中也存在问题,例如PG-SGA问题复杂、消耗时间较长,GLIM不同诊断标准内部之间一致性存在问题等。改良已有量表有助于国际化量表在国内更好的应用。
2.2.1 营养评估量表PG-SGA、mPG-SGA与abPG-SGA
PG-SGA是目前国际肿瘤患者营养评估时使用最广泛的工具[40],虽然其在中国已被广泛应用,但在实际应用过程中仍存在一些不足,例如量表操作复杂、耗费时间较长、对评估人员培训要求较高,而且不能区分营养良好与轻度营养不良。为了更加适应我国医疗环境,将国际问卷转化为适应中国人营养评估的问卷,中国抗癌协会肿瘤营养专委会改良了PG-SGA问卷,形成改良版患者主观整体评估(Modified PG-SGA, mPG-SGA),与经典PG-SGA相比,删除了50%以上专业人员认为难以完成和与总得分相关性<0.1的项目(包括体格检查、代谢及应激状态等),平均缩短1/3的问卷评估时间[41-43]。mPG-SGA检验效度、敏感度及特异性更好,并能分别预测营养良好和轻度营养不良患者的生存,比原版PG-SGA更好地预测患者生存[44-45]。mPG-SGA不但简便易行,而且其中不涉及专业问题,因此问题均可由患者自我作答,更有利于临床应用及传播。加拿大Gabrielson等提出了删减版患者主观整体评估(Abridged Patient-Generated Subjective Global Assessment, abPG-SGA),省略PG-SGA的第七部分体格检查不计,相较于PG-SGA更适用于门诊肿瘤患者,是门诊肿瘤患者营养状况评估的有效、实用、准确的工具[46]。
2.2.2 营养评估量表GLIM与量化GLIM
2018年发布的全球领导人营养不良倡议(Global leadership initiative on malnutrition, GLIM)是在营养风险筛查的基础上,利用表现型指标和病因性指标对患者营养不良急性评定和严重程度分级,对营养不良的定义和诊断标准进行了统一[23]。GLIM标准包括3个表型标准(非自主体重丢失、低BMI及肌肉量减少)和2个病因标准(摄食减少或消化吸收障碍,炎性反应或疾病负担)。GLIM有5个条目、6种组合,不同组合对同一人群得出的营养不良发生率差异很大。通过系统性分析各条目在肿瘤患者预后预测中的不同权重并进行量化评分,构建了全新的量化GLIM评分系统,有效解决了GLIM的局限性,有效对肿瘤患者营养不良及预后进行精准诊断和预测,量化GLIM评分系统诊断出的营养不良能够准确的在不同肿瘤以及相同肿瘤分期中区分出高死亡风险的患者,并为GLIM诊断工具的全球推广使用提供亚洲人群的证据。患者使用量化GLIM评估前无需营养筛查,用实际炎性反应符合水平代替肿瘤,预后预测效能显著提升,对于肿瘤患者综合治疗、改善预后具有重要临床意义[47-48]。
常见营养诊断工具虽然有较好的诊断效能,但其复杂程度同样阻碍了疾病患者获得营养工作者对自己营养状态的评估。随着临床工作的开展,不断改良、优化已有量表,在某种程度上比建立新量表更加有助于临床营养诊断工作的推进。
从2014年到2021年,我国恶性肿瘤住院患者营养不良发生率呈现一定的变化趋势,这为了解我国肿瘤患者营养不良的动态情况提供了数据支持[49],包括老年患者在内的恶性肿瘤患者的营养风险或营养不良患病率整体呈下降趋势,营养治疗率呈上升趋势。老年肿瘤患者的营养状况虽有所改善,但营养不良问题依然突出。胃癌、宫颈癌和恶性淋巴瘤等患者的营养风险或营养不良的患病率呈上升趋势,营养状况不容乐观,医务工作者应更加关注肿瘤患者的营养状况。时至今日,临床医生、患者及家属对明确营养治疗的适应证还存在很多误区,对肿瘤患者的营养管理还缺乏一定的规范性。未来有必要建立完善的营养治疗体系、规范营养管理、制定个性化治疗方案,为恶性肿瘤住院患者提供更好的营养治疗,从而改善其营养不良状况。
3 小结
我国肿瘤发病率和肿瘤患者数量逐年攀升。《“十四五”国民健康规划》中指出,要提高包括癌症在内的重大慢性病综合防治能力,强化预防、早期筛查和综合干预。基于此,围绕肿瘤患者的营养状况及营养不良的诊断与治疗开展了系统创新工作,探明我国肿瘤患者营养状况及关键问题,研究营养不良诊断新技术、营养治疗新模式及预后评价指标新体系,制定标准和指南、推广示范病房建设都有力促进了临床营养的发展及肿瘤治疗的进步与持续发展。
Competing interests: The authors declare that they have no competing interests.利益冲突声明:所有作者均声明不存在利益冲突。作者贡献:杨柳青:文献收集与整理,论文构思、设计、撰写与修改石汉平:论文指导与监督、审阅并修订 -
表 1 营养筛查工具AIWW问卷
Table 1 AIWW screening questionnaire
Questions Yes No Q1: Age (A)—Are you over 65 years old? □ □ Q2: Intake (I)—Have you noticed a decrease in appetite or food intake in the past month? □ □ Q3: Weight (W)—Did you lose your weight involuntarily over the past month? □ □ Q4: Walking (W)—Did your walking pace, walking steps, or walking distance decrease
involuntarily over the past month?□ □ Notes: Yes (add 1 point) or No (0 points). A score of 1 or more=patient is at risk of malnutrition. -
[1] Xu H, Song C, Yin L, et al. Extension protocol for the Investigation on Nutrition Status and Clinical Outcome of Patients with Common Cancers in China (INSCOC) study: 2021 update[J]. Precis Nutr, 2022, 7(2): 64-74.
[2] 郭树彬, 阮国添, 石汉平. 营养治疗是疾病的基础治疗、一线治疗[J]. 肿瘤代谢与营养电子杂志, 2024, 11(3): 308-313. [Guo SB, Ruan GT, Shi HP. Nutritional therapy is the basic treatment and first-line treatment of diseases[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2024, 11(3): 308-313.] Guo SB, Ruan GT, Shi HP. Nutritional therapy is the basic treatment and first-line treatment of diseases[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2024, 11(3): 308-313.
[3] Cederholm T, Barazzoni R, Austin P, et al. ESPEN guidelines on definitions and terminology of clinical nutrition[J]. Clin Nutr, 2017, 36(1): 49-64. doi: 10.1016/j.clnu.2016.09.004
[4] Mueller C, Compher C, Ellen DM. American Society for Parenteral and Enteral Nutrition (A. S. P. E. N. ) Board of Directors. A. S. P. E. N. clinical guidelines: Nutrition screening, assessment, and intervention in adults[J]. JPEN J Parenter Enteral Nutr, 2011, 35(1): 16-24. doi: 10.1177/0148607110389335
[5] 石汉平, 赵青川, 王昆华, 等. 营养不良的三级诊断[J]. 肿瘤代谢与营养电子杂志, 2015, 2(2): 31-36. [Shi HP, Zhao QC, Wang KH, et al. Three-level Diagnosis of Malnutrition[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2015, 2(2): 31-36.] Shi HP, Zhao QC, Wang KH, et al. Three-level Diagnosis of Malnutrition[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2015, 2(2): 31-36.
[6] Yang B, Wang L, Yu K, et al. Three-Stage Nutrition Diagnosis for surgical patients at the perioperative period[J]. Eur J Surg Oncol, 2024, 50(5): 106759. doi: 10.1016/j.ejso.2022.10.019
[7] Yang HC, Thornton LM, Shapiro CL. Surviving recurrence: psychological and quality-of-life recovery[J]. Cancer, 2008, 112(5): 1178-1187. doi: 10.1002/cncr.23272
[8] 中国抗癌协会肿瘤营养专业委员会, 国家市场监管重点实验室(肿瘤特医食品), 中国营养保健食品协会特殊医学用途配方食品应用委员会. 规范化外科营养诊疗示范病房标准[J]. 肿瘤代谢与营养电子杂志, 2022, 9(2): 175-184. [Chinese Society of Nutritional Oncology, Key Laboratory of Cancer FSMP for State Market Regulation, Formula Food for Special Medical Purposes Application Committee, China Nutrition and Health Food Association. Standards of standardized surgical nutritional diagnosis and treatment ward[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2022, 9(2): 175-184.] doi: 10.3969/j.issn.2095-7807.2022.2.zldxyyy202202008 Chinese Society of Nutritional Oncology, Key Laboratory of Cancer FSMP for State Market Regulation, Formula Food for Special Medical Purposes Application Committee, China Nutrition and Health Food Association. Standards of standardized surgical nutritional diagnosis and treatment ward[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2022, 9(2): 175-184. doi: 10.3969/j.issn.2095-7807.2022.2.zldxyyy202202008
[9] 石汉平, 许红霞, 李苏宜, 等. 营养不良的五阶梯治疗[J]. 肿瘤代谢与营养电子杂志, 2015, 2(1): 29-33. [Shi HP, Xu HX, Li SY, et al. The Five-step Treatment for Malnutrition[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2015, 2(1): 29-33.] Shi HP, Xu HX, Li SY, et al. The Five-step Treatment for Malnutrition[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2015, 2(1): 29-33.
[10] 王林, 丛明华, 崔久嵬, 等. 肿瘤营养治疗的基本原则[J]. 肿瘤代谢与营养电子杂志, 2022, 9(6): 727-734. [Wang L, Cong MH, Cui JW, et al. Principles in cancer nutrition therapy[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2022, 9(6): 727-734.] Wang L, Cong MH, Cui JW, et al. Principles in cancer nutrition therapy[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2022, 9(6): 727-734.
[11] 吴燕, 方红梅. 新型冠状病毒肺炎患者的个体化营养支持治疗[J]. 中国现代应用药学, 2020, 37(4): 394-397. [Wu Y, Fang HM. Individualized nutritional support therapeutics for patients with COVID-19[J]. Zhongguo Xian Dai Ying Yong Yao Xue, 2020, 37(4): 394-397.] Wu Y, Fang HM. Individualized nutritional support therapeutics for patients with COVID-19[J]. Zhongguo Xian Dai Ying Yong Yao Xue, 2020, 37(4): 394-397.
[12] 孙欣彤, 田英梅. 五阶梯治疗在老年营养不良患者中的应用分析[J]. 中外医疗, 2019, 38(21): 139-142. [Sun XT, Tian YM. Application analysis of five-step treatment in elderly patients with mal-nutrition[J]. Zhong Wai Yi Liao, 2019, 38(21): 139-142.] Sun XT, Tian YM. Application analysis of five-step treatment in elderly patients with mal-nutrition[J]. Zhong Wai Yi Liao, 2019, 38(21): 139-142.
[13] 王宗秋, 高成, 常飞, 等. 五阶梯治疗在老年营养不良患者中的应用分析[J]. 医学食疗与健康, 2020, 18(12): 6, 10. [Wang ZQ, Gao C, Chang F, et al. Analysis on the Application of the Five-step Treatment in Elderly Patients with Malnutrition[J]. Yi Xue Shi Liao Yu Jian Kang, 2020, 18(12): 6, 10.] Wang ZQ, Gao C, Chang F, et al. Analysis on the Application of the Five-step Treatment in Elderly Patients with Malnutrition[J]. Yi Xue Shi Liao Yu Jian Kang, 2020, 18(12): 6, 10.
[14] 石汉平, 李增宁, 王昆华, 等. 营养管理新模式—HCH[J]. 肿瘤代谢与营养电子杂志, 2015, 2(3): 23-26. [Shi HP, Li ZN, Wang KH, et al. New models of nutrition management—HCH[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2015, 2(3): 23-26.] Shi HP, Li ZN, Wang KH, et al. New models of nutrition management—HCH[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2015, 2(3): 23-26.
[15] 顾文英, 章滨云, 董枫, 等. 肿瘤整合康复管理专家共识(2024)[J]. 健康发展与政策研究, 2024, 27(3): 275-284. [Gu WY, Zhang BY, Dong F, et al. Expert consensus on tumor integrated rehabilitation management(2024)[J]. Jian Kang Fa Zhan Yu Zheng Ce Yan Jiu, 2024, 27(3): 275-284.] doi: 10.12458/HDPR.202407065 Gu WY, Zhang BY, Dong F, et al. Expert consensus on tumor integrated rehabilitation management(2024)[J]. Jian Kang Fa Zhan Yu Zheng Ce Yan Jiu, 2024, 27(3): 275-284. doi: 10.12458/HDPR.202407065
[16] 李红侠, 张其德, 凌亭生, 等. 医院-家庭营养管理模式联合激励式护理干预在早期消化道肿瘤内镜手术患者中的应用[J]. 中国临床研究, 2024, 37(9): 1458-1462, 1466. [Li HX, Zhang QD, Ling TS, et al. Effects of hospital-to-home nutritional management model combined with motivational care intervention in patients undergoing endoscopic surgery for early gastrointestinal tumors[J]. Zhongguo Lin Chuang Yan Jiu, 2024, 37(9): 1458-1462, 1466.] Li HX, Zhang QD, Ling TS, et al. Effects of hospital-to-home nutritional management model combined with motivational care intervention in patients undergoing endoscopic surgery for early gastrointestinal tumors[J]. Zhongguo Lin Chuang Yan Jiu, 2024, 37(9): 1458-1462, 1466.
[17] 胡于琴, 陈雯, 江海燕, 等. H2H营养管理模式在稳定期炎症性肠病患者中的应用研究[J]. 中国临床护理, 2024, 16(5): 290-292,296. [Hu YQ, Chen W, Jiang HY, et al. Application of H2H nutrition management in IBD patients[J]. Zhongguo Lin Chuang Hu Li, 2024, 16(5): 290-292, 296.] doi: 10.3969/j.issn.1674-3768.2024.05.007 Hu YQ, Chen W, Jiang HY, et al. Application of H2H nutrition management in IBD patients[J]. Zhongguo Lin Chuang Hu Li, 2024, 16(5): 290-292, 296. doi: 10.3969/j.issn.1674-3768.2024.05.007
[18] 周岚, 徐骞. 医院-社区-家庭跟进式营养管理模式对胃癌术后患者营养状况及生存质量的影响[J]. 西藏医药, 2024, 45(2): 71-72. [Zhou L, Xu Q. Impact of the hospital-community-family follow-up nutrition management model on the nutritional status and quality of life of patients after gastric cancer surgery[J]. Xizang Yi Yao, 2024, 45(2): 71-72.] Zhou L, Xu Q. Impact of the hospital-community-family follow-up nutrition management model on the nutritional status and quality of life of patients after gastric cancer surgery[J]. Xizang Yi Yao, 2024, 45(2): 71-72.
[19] Zhao R, Hou X, Niu Y, et al. Effect of the Home to Hospital to Home nutrition management program on postoperative liver cancer patients: A single-center randomized controlled study[J]. Medicine (Baltimore), 2023, 102(49): e36648. doi: 10.1097/MD.0000000000036648
[20] Obling SR, Wilson BV, Pfeiffer P, et al. Home parenteral nutrition increases fat free mass in patients with incurable gastrointestinal cancer. Results of a randomized controlled trial[J]. Clin Nutr, 2019, 38(1): 182-190. doi: 10.1016/j.clnu.2017.12.011
[21] Marshall AP, Tobiano G, Roberts S, et al. End-user perceptions of a patient- and family-centred intervention to improve nutrition intake among oncology patients: a descriptive qualitative analysis[J]. BMC Nutr, 2020, 6: 29. doi: 10.1186/s40795-020-00353-8
[22] Amano K, Maeda I, Ishiki H, et al. East-Asian collaborative cross-cultural Study to Elucidate the Dying process (EASED) Investigators. Effects of enteral nutrition and parenteral nutrition on survival in patients with advanced cancer cachexia: Analysis of a multicenter prospective cohort study[J]. Clin Nutr, 2021, 40(3): 1168-1175. doi: 10.1016/j.clnu.2020.07.027
[23] Cederholm T, Jensen GL, Correia MITD, et al. GLIM Core Leadership Committee, GLIM Working Group. GLIM criteria for the diagnosis of malnutrition - A consensus report from the global clinical nutrition community[J]. J Cachexia Sarcopenia Muscle, 2019, 10(1): 207-217. doi: 10.1002/jcsm.12383
[24] Cederholm T, Bosaeus I, Barazzoni R, et al. Diagnostic criteria for malnutrition - An ESPEN Consensus Statement[J]. Clin Nutr, 2015, 34(3): 335-340. doi: 10.1016/j.clnu.2015.03.001
[25] Tan S, Jiang J, Qiu L, et al. Prevalence of Malnutrition in Patients with Hepatocellular Carcinoma: A Comparative Study of GLIM Criteria, NRS2002, and PG-SGA, and Identification of Independent Risk Factors[J]. Nutr Cancer, 2024, 76(4): 335-344. doi: 10.1080/01635581.2024.2314317
[26] Ge YZ, Fu ZM, Zhang Q, et al. Investigation on Nutrition Status and Clinical Outcome of Common Cancers (INSCOC) Group. AIWW: a new nutrition-screening tool for the oncologic population[J]. Sci China Life Sci, 2023, 66(8): 1831-1840. doi: 10.1007/s11427-022-2292-9
[27] Siegel RL, Miller KD, Wagle NS, et al. Cancer statistics, 2023[J]. CA Cancer J Clin, 2023, 73(1): 17-48. doi: 10.3322/caac.21763
[28] Duymus ME, Ugur M, Dal MB, et al. Prognostic value of Prognostic Nutritional Index (PNI) for 5-year recurrence-free survival in surgically resected gastrointestinal stromal tumors[J]. Ann Ital Chir, 2023, 94: 19-26.
[29] Zhang Z, Wan Z, Zhu Y, et al. Prevalence of malnutrition comparing NRS2002, MUST, and PG-SGA with the GLIM criteria in adults with cancer: A multi-center study[J]. Nutrition, 2021, 83: 111072. doi: 10.1016/j.nut.2020.111072
[30] Shi J, Liu T, Ge Y, et al. Cholesterol-modified prognostic nutritional index (CPNI) as an effective tool for assessing the nutrition status and predicting survival in patients with breast cancer[J]. BMC Med, 2023, 21(1): 512. doi: 10.1186/s12916-023-03225-7
[31] Xie H, Ruan G, Ge Y, et al. Inflammatory burden as a prognostic biomarker for cancer[J]. Clin Nutr, 2022, 41(6): 1236-1243. doi: 10.1016/j.clnu.2022.04.019
[32] Tan CS, Read JA, Phan VH, et al. The relationship between nutritional status, inflammatory markers and survival in patients with advanced cancer: a prospective cohort study[J]. Support Care Cancer, 2015, 23(2): 385-391. doi: 10.1007/s00520-014-2385-y
[33] He C, Wu D, Wei X, et al. Association between inflammatory burden index and all-cause mortality in the general population aged over 45 years: Data from NHANES 2005-2017[J]. Nutr Metab Cardiovasc Dis, 2024, 34(1): 64-74. doi: 10.1016/j.numecd.2023.10.006
[34] Du M, Xu L, Zhang X, et al. Association Between Inflammatory Burden Index and Unfavorable Prognosis After Endovascular Thrombectomy in Acute Ischemic Stroke[J]. J Inflamm Res, 2023, 16: 3009-3017. doi: 10.2147/JIR.S419087
[35] Song R, Ni H, Huang J, et al. Prognostic Value of Inflammation-Immunity-Nutrition Score and Inflammatory Burden Index for Hepatocellular Carcinoma Patients After Hepatectomy[J]. J Inflamm Res, 2022, 15: 6463-6479. doi: 10.2147/JIR.S386407
[36] 吴小林, 贺丹, 龚红霞, 等. GLIM标准与PG-SGA在肿瘤患者营养不良诊断中的应用[J]. 肿瘤代谢与营养电子杂志, 2021, 8(4): 403-407. [Wu XD, He D, Gong HX, et al. Application of global leadership initiative on malnutrition and patient?generated subjective global assessment in diagnosing malnutrition among cancer patients[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2021, 8(4): 403-407.] Wu XD, He D, Gong HX, et al. Application of global leadership initiative on malnutrition and patient?generated subjective global assessment in diagnosing malnutrition among cancer patients[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2021, 8(4): 403-407.
[37] Henriksen C, Paur I, Pedersen A, et al. Agreement depends on the screening tool used in GLIM[J]. Clin Nutr, 2022, 41(2): 329-336. doi: 10.1016/j.clnu.2021.12.024
[38] Balcı C, Tufan G, Özdemir N, et al. GLIM criteria as a valid tool for nutrition assessment and mortality prediction in treatment-naïve patients with cancer[J]. Nutr Clin Pract, 2023, 38(4): 798-806. doi: 10.1002/ncp.10969
[39] Sheas MN, Ali SR, Safdar W, et al. Nutritional Assessment in Cancer Patients[J]. Cancer Treat Res, 2023, 185: 285-310.
[40] Jager-Wittenaar H, Ottery FD. Assessing nutritional status in cancer: role of the Patient-Generated Subjective Global Assessment[J]. Curr Opin Clin Nutr Metab Care, 2017, 20(5): 322-329. doi: 10.1097/MCO.0000000000000389
[41] 张芮, 冯瑞珂, 付振明. 中国版患者主观整体评估: 最可能实现肿瘤患者营养状况自我评估的工具[J]. 肿瘤代谢与营养电子杂志, 2023, 10(3): 325-329. [Zhang R, Feng RK, Fu ZM. Chinese version of patient-generated subjective global assessment: the most likely tool to achieve self-assessment of nutritional status of cancer patients[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2023, 10(3): 325-329.] Zhang R, Feng RK, Fu ZM. Chinese version of patient-generated subjective global assessment: the most likely tool to achieve self-assessment of nutritional status of cancer patients[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2023, 10(3): 325-329.
[42] Huo Z, Chong F, Yin L, et al. Investigation on Nutrition Status and Clinical Outcome of Common Cancers (INSCOC) Group. Comparison of the performance of the GLIM criteria, PG-SGA and mPG-SGA in diagnosing malnutrition and predicting survival among lung cancer patients: A multicenter study[J]. Clin Nutr, 2023, 42(6): 1048-1058. doi: 10.1016/j.clnu.2023.04.021
[43] Fu Z, Zhang R, Wang KH, et al. Development and validation of a Modified Patient-Generated Subjective Global Assessment as a nutritional assessment tool in cancer patients[J]. J Cachexia Sarcopenia Muscle, 2022, 13(1): 343-354. doi: 10.1002/jcsm.12872
[44] 苏文意, 李波, 姜祺澜, 等. 改良版患者主观整体评估可用于原发性肝癌患者营养不良的评估[J]. 肿瘤代谢与营养电子杂志, 2024, 11(3): 360-366. [Su WY, Li B, Jiang QL, et al. The modified patient-generated subjective global assessment can be used for the assessment of malnutrition in patients with primary liver cancer[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2024, 11(3): 360-366.] Su WY, Li B, Jiang QL, et al. The modified patient-generated subjective global assessment can be used for the assessment of malnutrition in patients with primary liver cancer[J]. Zhong Liu Dai Xie Yu Ying Yang Dian Zi Za Zhi, 2024, 11(3): 360-366.
[45] Chong F, Huo Z, Yin L, et al. Value of the modified Patient-Generated Subjective Global Assessment in indicating the need for nutrition intervention and predicting overall survival in patients with malignant tumors in at least two organs[J]. Nutr Clin Pract, 2024, 39(4): 920-933. doi: 10.1002/ncp.11140
[46] Gabrielson DK, Scaffidi D, Leung E, et al. Use of an abridged scored Patient-Generated Subjective Global Assessment (abPG-SGA) as a nutritional screening tool for cancer patients in an outpatient setting[J]. Nutr Cancer, 2013, 65(2): 234-239. doi: 10.1080/01635581.2013.755554
[47] Zhang Q, Zhang KP, Zhang X, et al. Scored-GLIM as an effective tool to assess nutrition status and predict survival in patients with cancer[J]. Clin Nutr, 2021, 40(6): 4225-4233. doi: 10.1016/j.clnu.2021.01.033
[48] Luo X, Cai B, Jin W. A modified GLIM criteria-based nomogram for the survival prediction of gastric cancer patients undergoing surgical resection[J]. BMC Gastroenterol, 2024, 24(1): 307. doi: 10.1186/s12876-024-03395-5
[49] Zhou M, Xu H, Cui Ji, et al. Variation trends of malnutrition status among malignancy inpatients in China from 2014 to 2021[J]. Precis Nutr, 2023, 2(1): e00028.



 石汉平: 医学博士,教授,主任医师,博士生导师。首都医科大学附属北京世纪坛医院普外四科主任、肿瘤营养与代谢中心主任。国家市场监管重点实验室(肿瘤特医食品)主任,肿瘤代谢与营养北京国际科技合作基地主任。国家重点研发计划项目首席科学家。北京市战略人才及团队带头人。美国外科学院院士(FACS)。以第一获奖人获省部级科技进步一等奖3项、二等奖2项。Journal of Nutritional Oncology主编;Precision Nutrition主编;《医学参考报—营养学专刊》主编;《肿瘤代谢与营养电子杂志》主编;中国抗癌协会副理事长;中国营养保健食品协会副会长;中国抗癌协会肿瘤营养专业委员会主任委员;国民营养健康专家委员会临床营养行动专业委员会主任委员;中国食品科学技术学会医学食品分会主任委员
。
石汉平: 医学博士,教授,主任医师,博士生导师。首都医科大学附属北京世纪坛医院普外四科主任、肿瘤营养与代谢中心主任。国家市场监管重点实验室(肿瘤特医食品)主任,肿瘤代谢与营养北京国际科技合作基地主任。国家重点研发计划项目首席科学家。北京市战略人才及团队带头人。美国外科学院院士(FACS)。以第一获奖人获省部级科技进步一等奖3项、二等奖2项。Journal of Nutritional Oncology主编;Precision Nutrition主编;《医学参考报—营养学专刊》主编;《肿瘤代谢与营养电子杂志》主编;中国抗癌协会副理事长;中国营养保健食品协会副会长;中国抗癌协会肿瘤营养专业委员会主任委员;国民营养健康专家委员会临床营养行动专业委员会主任委员;中国食品科学技术学会医学食品分会主任委员
。
 下载:
下载:

