Establishment of Risk-Prediction Model for Axillary Lymph-Node Metastasis in Microinvasive Breast Cancer Based on SEER Database
-
摘要:目的
分析微浸润乳腺癌(MIBC)患者腋窝淋巴结转移(ALNM)的影响因素,构建MIBC患者同侧ALNM风险预测模型。
方法通过SEER数据库检索并筛选出2010—2015年病理确诊的
4475 例原发MIBC女性患者作为建模组,另筛选SEER数据库中2018—2020年病理确诊的2266 例原发MIBC女性患者作为外部验证组,收集入组MIBC患者的临床病理资料,单因素分析筛选出影响MIBC患者ALNM的因素,将有统计学意义的变量纳入多因素Logistic回归分析,筛选出影响MIBC患者ALNM的独立影响因子并建立列线图,绘制受试者工作特征(ROC)曲线计算曲线下面积(AUC),绘制校准曲线,并行Hosmer-Lemeshow拟合优度检验进行模型评价。结果纳入
6741 例MIBC患者中发生同侧ALNM患者为309例,比例约为4.58%。建模组单因素分析显示:年龄、种族、组织学分级、病理类型、分子亚型、边侧与MIBC患者ALNM相关(P<0.05)。多因素分析结果显示:≤40岁、黑种人、组织学分级Ⅱ级及Ⅲ级、原发于右侧的MIBC发生ALNM的风险更高(P<0.05),分子亚型是MIBC患者ALNM的独立影响因素,但HR+HER2+、HR−HER2+、HR−HER2−三种分子亚型MIBC与HR+HER2−亚型间ALNM风险差异均无统计学意义。利用上述变量建立预测列线图,得出建模组AUC为0.716,(95%CI: 0.682~0.750),最佳截断值为0.045,其敏感度为0.733,特异性为0.608。将新建的列线图模型用于验证组,其AUC为0.722(95%CI: 0.667~0.777)。建模组及验证组的校准曲线Hosmer-Lemeshow拟合优度检验均P>0.05。结论通过SEER数据库建立的MIBC患者ALNM风险预测模型,预测能力较好,有望为临床实践提供参考。
Abstract:ObjectiveTo analyze the factors influencing axillary lymph-node metastasis (ALNM) in microinvasive breast cancer (MIBC) patients, as well as to establish the risk-prediction model of ipsilateral ALNM in MIBC patients.
MethodsA total of 4475 primary female MIBC diagnosed by pathology from 2010 to 2015 were searched and screened from the SEER database. The obtained data were used to establish a prediction model for ALNM of MIBC. A total of 2266 primary female MIBC patients diagnosed by pathology from 2018 to 2020 in the SEER database were screened as the external validation cohort. The clinicopathological data of the enrolled MIBC patients were collected. Univariate analysis was used to screen out the factors affecting ALNM in MIBC patients. Statistically significant variables in univariate analysis were included in multivariate logistic regression analysis. The independent factors influencing ALNM in MIBC patients were screened out, and a nomogram was established. The area under the curve (AUC) was calculated by plotting the ROC curve. After plotting the calibration curve, the model was evaluated by Hosmer-Lemeshow goodness-of-fit test.
ResultsA total of 309 patients were diagnosed with ipsilateral ALNM among the 6741 MIBC patients, accounting for about 4.58%. Univariate analysis of the modeling group showed that age, ethnicity, histological grade, pathological type, molecular subtype, and lateral side were associated with ALNM in MIBC patients (P<0.05). Results of multivariate analysis showed that the risk of ALNM was higher in MIBC patients ≤40 years old, black people, histological grade Ⅱ and Ⅲ, and primary right side (P<0.05). Subtype is an independent factor influencing ALNM in MIBC patients. However, the difference in ALNM risk was not statistically significant between the subtype of HR+HER2+, HR−HER2+, HR−HER2− and HR+HER2− subtypes. The AUC of the modeling group was 0.716 (95%CI: 0.682-0.750), the best cut-off value was 0.045, the sensitivity was 0.733, and the specificity was 0.608. The newly established nomogram model was used for the validation cohort, and its AUC was 0.722 (95%CI: 0.667-0.777). The P values of the Hosmer-Lemeshow goodness-of-fit test of the calibration curves in the modeling and validation groups exceeded 0.05.
ConclusionThe risk-prediction model of ALNM in MIBC patients established by the SEER database has good predictive ability and can thus be expected to serve as a reference for clinical practice.
-
0 引言
乳腺癌已成为全球范围内女性发病率第一位的恶性肿瘤[1]。微浸润乳腺癌(microinvasive breast cancer, MIBC)的定义经历过很长一段时间的争议,1997年美国癌症联合委员会(AJCC)提出MIBC的定义是指乳腺间质中肿瘤细胞浸润灶的最大径≤1 mm[2],得到了广泛认可并沿用至今。MIBC在乳腺癌中的比例为0.68%~3.4%[3]。MIBC发生腋窝淋巴结转移(axillary lymph node metastasis, ALNM)的比例较少,约为2.9%[4]。虽然MIBC伴同侧ALNM概率较低,但基于乳腺癌较高的发病率,临床实践中MIBC伴同侧ALNM的患者并不少见。由于较低的ALNM率,是否需要对所有MIBC患者常规行腋窝前哨淋巴结活检一直以来争议不断[5-7],若能根据临床病理特征预测MIBC患者ALNM风险,可协助临床医生评估腋窝淋巴结状态,对MIBC患者是否行前哨淋巴结活检(sentinel lymph node biopsy, SLNB)个体化处理,目前仍缺乏MIBC患者ALNM的预测模型。本研究通过收集SEER数据库MIBC患者的临床病理资料,建立MIBC患者ALNM预测模型,希望可以协助临床医生更好地评估MIBC患者腋窝淋巴结是否转移。
1 资料与方法
1.1 数据来源及入组标准
本研究建模组数据来自SEER数据库(SEER Research Plus Data, 17 Registries, Nov 2021 Sub(2000—2019))。通过SEER*Stat 8.4.2软件从SEER数据库获取2010—2015年4 523例原发性乳腺癌患者的病历资料,所有患者根据AJCC第7版T分期分为T1mic期,不合并其他器官原发恶性肿瘤,排除男性、双侧乳腺癌、叶状肿瘤、存在远处转移、病历资料不完整或未经病理证实的患者,最终纳入4 475例作为建模组。外部验证组数据来自SEER数据库(SEER Research Data, 17 Registries, Nov 2022 Sub(2000—2020)),通过SEER*Stat 8.4.2软件从SEER数据库获取2018—2020年
2294 例原发性乳腺癌患者的病历资料,所有患者根据第8版疾病程度(extent of disease, EOD)分期T分期为T1mic期,不合并其他器官原发恶性肿瘤,排除男性、双侧乳腺癌、边侧不明、存在远处转移、病历资料不完整或未经病理证实的患者,最终纳入2 266例作为外部验证组。1.2 统计学方法
计数资料用频数和百分比表示。变量的选择主要依据临床实践中可能影响乳腺癌ALNM的因素及既往文献报道的因素,单因素分析采用卡方检验或Fisher’s精确检验,将单因素分析有统计学意义的变量或既往研究证实与之相关的变量纳入多因素分析,多因素分析采用二元Logistic回归分析,统计分析均应用SPSS25软件。AUC计算及列线图、ROC曲线、校准曲线的绘制均采用R4.2.2软件,R4.2.2软件包“regplot”绘制列线图,应用“pROC”和“rms”包绘制ROC曲线、校准曲线并计算AUC及其95%CI。P<0.05为差异有统计学意义。Hosmer-Lemeshow检验进行拟合优度检验,P>0.05表明模型预测值与实际值无明显差异,模型拟合良好。
2 结果
2.1 研究对象临床病理资料
本研究共纳入
6741 例MIBC患者,年龄21岁以上,中位年龄58岁。其中发生同侧ALNM的患者为309例,约4.58%,年龄范围23~92岁,中位年龄51岁。其中建模组中发生ALNM的患者为225例(225/4475 ,5.03%),年龄范围28~92岁,中位年龄51岁。验证组中发生ALNM的患者为84例(84/2266 ,3.71%),年龄范围23~84岁,中位年龄52岁。入组患者临床病理资料见表1。表 1 微浸润乳腺癌患者临床病理资料[n(%)]Table 1 Clinicopathological data of MIBC patients (n (%))Characteristics Training
cohort
(n=4475)Validation
cohort
(n=2266)Total
(n=6741)Age(years) ≤40 270(6.03) 149(6.58) 419(6.22) 41-60 2364(52.83) 1066(47.04) 3430(50.88) 61-80 1684(37.63) 988(43.60) 2672(39.64) ≥81 157(3.51) 63(2.78) 220(3.26) Race White 3307(73.90) 1543(68.09) 4850(71.95) Black 517(11.55) 279(12.31) 796(11.81) Others/
Unknown651(14.55) 444(19.59) 1095(16.24) Grade Ⅰ 768(17.16) 399(17.61) 1167(17.31) Ⅱ 1223(27.33) 538(23.74) 1761(26.12) Ⅲ 867(19.37) 215(9.49) 1082(16.05) Ⅳ 44(0.98) 2(0.09) 46(0.68) Unknown 1573(35.15) 1112(49.07) 2685(39.83) Histologic type IDC 3919(87.58) 2043(90.16) 5962(88.44) Others 556(12.42) 223(9.84) 779(11.56) Subtype HR+HER2− 1604(35.84) 939(41.44) 2543(37.72) HR+HER2+ 503(11.24) 232(10.24) 735(10.90) HR−HER2+ 468(10.46) 235(10.37) 703(10.43) HR−HER2− 236(5.27) 110(4.85) 346(5.13) Unknown 1664(37.18) 750(33.10) 2414(35.81) Primary site
(quadrant of
breast)Upper-outer 1559(34.84) 755(33.32) 2314(34.33) Lower-outer 314(7.02) 199(8.78) 513(7.61) Upper-inner 471(10.53) 234(10.33) 705(10.46) Lower-inner 302(6.75) 147(6.49) 449(6.67) Central portion 226(5.05) 145(6.40) 371(5.50) Axillary tail 16(0.36) 6(0.26) 22(0.33) Overlapping
lesion949(21.21) 550(24.27) 1499(22.24) Nipple 14(0.31) 6(0.26) 20(0.30) Breast, NOS 624(13.94) 224(9.89) 848(12.58) Marital status Married 2723(60.85) 1405(62.00) 4128(61.24) Unmarried 1516(33.88) 760(33.54) 2276(33.76) Unknown 236(5.27) 101(4.46) 337(5.00) Laterality(origin
of primary)Left 2330(52.07) 1189(52.47) 3519(52.20) Right 2145(47.93) 1077(47.53) 3222(47.80) N N0 4250(94.97) 2182(96.29) 6432(95.42) N+ 225(5.03) 84(3.71) 309(4.58) Notes: MIBC: microinvasive breast cancer; Grade Ⅳ: undifferentiated; N: Ipsilateral axillary lymph nodes; N+: positive axillary lymph nodes; IDC: infiltrating duct carcinoma; Unmarried included single (never married), divorced, separated, widowed, domestic partner; NOS: not otherwise specified. 2.2 建模组ALNM影响因素分析
建模组同侧腋窝淋巴结转移的单因素分析,见表2。年龄、种族、组织学分级、病理类型、分子亚型、边侧与MIBC患者ALNM有关(P<0.05)。肿瘤位置、婚姻状态与MIBC患者ALNM无关(P>0.05)。将单因素分析有统计学意义的变量纳入多因素Logistic回归分析,其结果显示:≤40岁、黑种人、组织学分级Ⅱ级及Ⅲ级、原发于右侧的乳腺癌发生腋窝淋巴结转移的风险更高(P<0.05),分子亚型是MIBC患者ALNM的独立影响因素,但HR+HER2+、HR−HER2+、HR−HER2−三种分子亚型MIBC与HR+HER2−亚型间ALNM风险差异均无统计学意义,见表3。
表 2 MIBC患者ALNM的单因素分析Table 2 Univariate analysis of ALNM in MIBC patientsCharacteristics N0 N+ χ2 or Fisher P Age(years) 57.386 <0.001 ≤40 236 34 41-60 2223 141 61-80 1639 45 ≥81 152 5 Race 10.118 0.006 White 3147 160 Black 477 40 Others/Unknown 626 25 Grade 38.198 <0.001 Ⅰ 748 20 Ⅱ 1160 63 Ⅲ 791 76 Ⅳ 43 1 Unknown 1508 65 Histologic type 5.162 0.023 IDC 3711 208 Others 539 17 Subtype 46.027 <0.001 HR+HER2− 1527 77 HR+HER2+ 459 44 HR−HER2+ 432 36 HR−HER2− 215 21 Unknown 1617 47 Primary Site
(quadrant of breast)12.588 0.109 Upper-outer 1485 74 Lower-outer 304 10 Upper-inner 453 18 Lower-inner 289 13 Central portion 214 12 Axillary tail 15 1 Overlapping lesion 900 49 Nipple 13 1 Breast, NOS 577 47 Marital status 4.703 0.095 Married 2596 127 Unmarried 1426 90 Unknown 228 8 Laterality
(origin of primary)6.877 0.009 Left 2232 98 Right 2018 127 Note: ALNM: axillary lymph node metastasis. 表 3 MIBC患者ALNM的多因素Logistic回归分析Table 3 Multivariate Logistic regression analysis of ALNM in MIBC patientsCharacteristics OR 95%CI P Age(years) <0.001 ≤40 1 41-60 0.460 0.306-0.692 <0.001 61-80 0.214 0.132-0.346 <0.001 ≥81 0.251 0.095-0.665 <0.001 Race 0.014 White 1 Black 1.537 1.061-2.226 0.023 Others/Unknown 0.727 0.469-1.125 0.152 Grade <0.001 Ⅰ 1 Ⅱ 1.720 1.019-2.905 0.042 Ⅲ 2.917 1.707-4.985 <0.001 Ⅳ 0.830 0.106-6.491 0.859 Unknown 1.533 0.901-2.606 0.115 Subtype <0.001 HR+HER2− 1 HR+HER2+ 1.329 0.887-1.992 0.168 HR−HER2+ 1.082 0.696-1.681 0.726 HR−HER2− 1.493 0.882-2.528 0.136 Unknown 0.477 0.324-0.700 <0.001 Laterality(origin of primary) 0.013 Left 1 Right 1.420 1.077-1.871 0.013 2.3 建立MIBC患者ALNM列线图预测模型
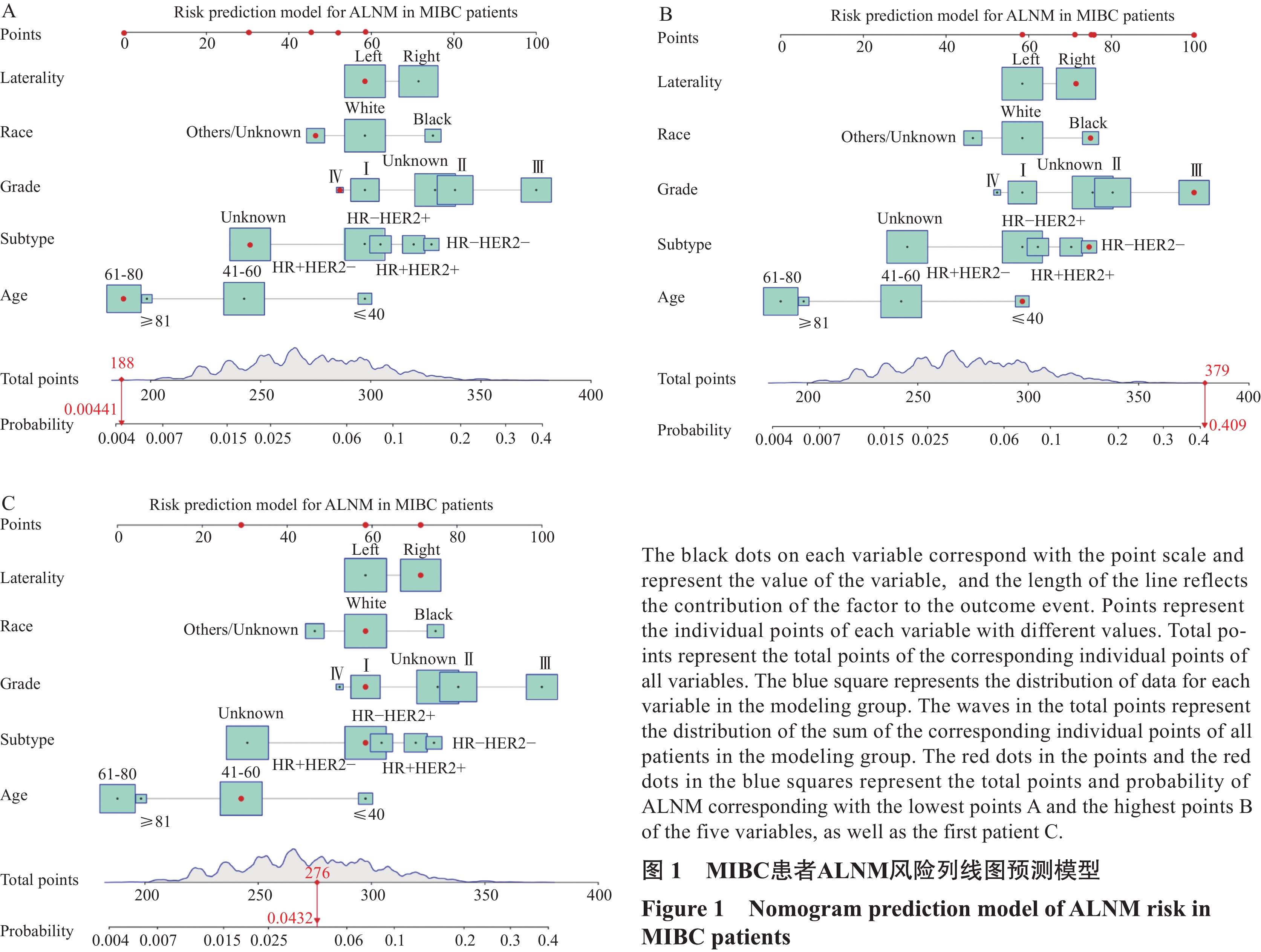
将MIBC患者ALNM的独立影响因素进行列线图的绘制,得出MIBC患者ALNM的预测模型,每一个影响因素对应分值标尺得出分数后,将这些分数相加得出总分,对应得出列线图下方的ALNM风险。本研究建模组建立的列线图中年龄、分子分型、组织学分级对ALNM的分值占比更大,其次是种族,而边侧对ALNM的分值占比最小。当建模组患者的边侧、种族、组织学分级、分子亚型及年龄对应分值均为最低时,其对应的总分为188,对应的ALNM概率为0.441%,见图1A。如上述指标对应的分值均为最高值时,其对应的总分为379,对应的ALNM概率为40.9%,见图1B。本研究建立的列线图可以评估MIBC患者ALNM概率的范围为0.441%~40.9%。对于此列线图的使用以建模组第1例患者为例,该患者的总分为276,其ALNM概率约为4.32%,见图1C。
2.4 预测模型的评价与验证
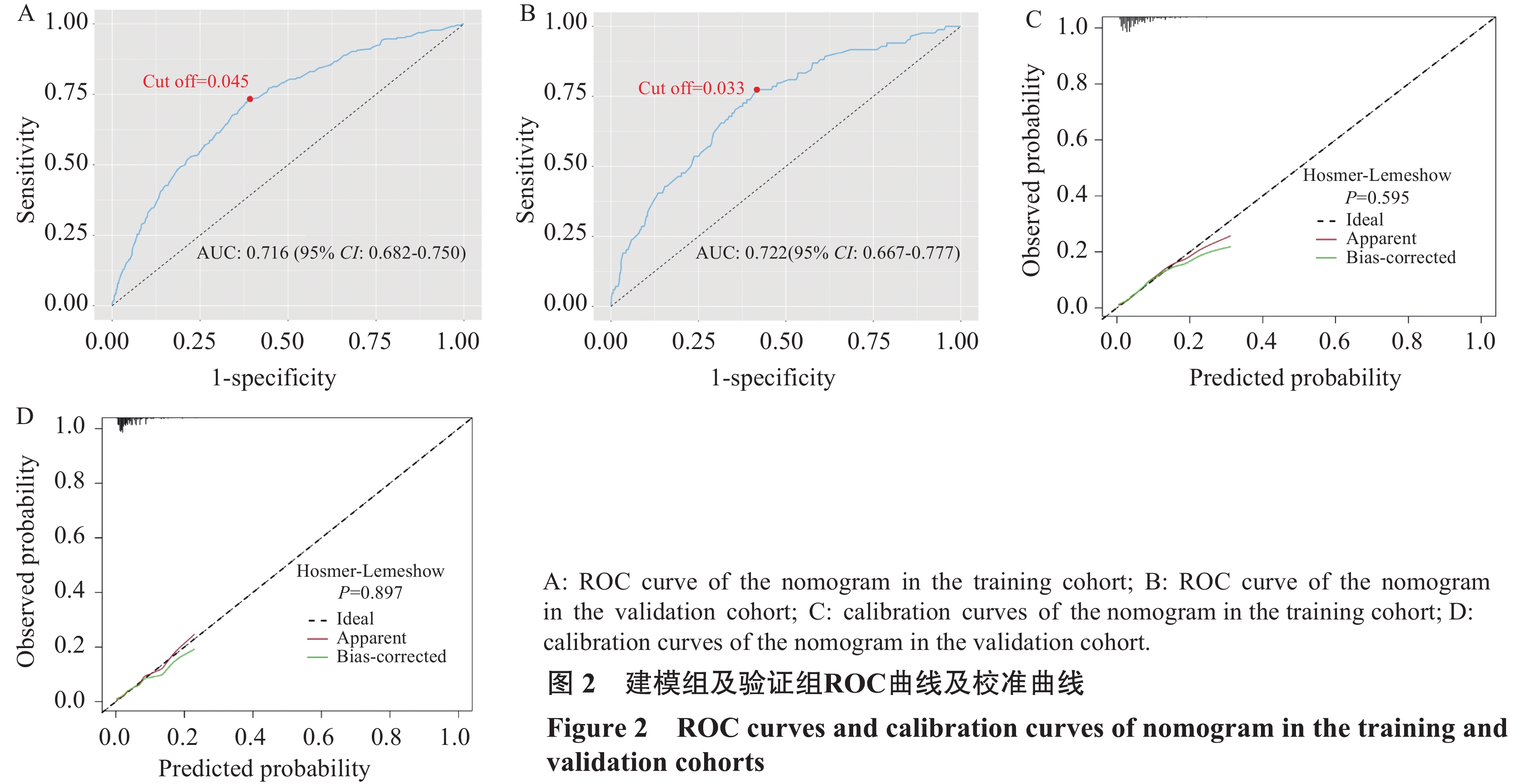
通过绘制ROC曲线,根据其AUC来评价预测模型。建模组的AUC为0.716(95%CI: 0.682~0.750),最佳截断值为0.045,相应敏感度为0.733,特异度为0.608,见图2A。验证组AUC为0.722(95%CI: 0.667~0.777),最佳截断值为0.033,相应敏感度为0.774,特异度为0.583,见图2B。同时绘制校正曲线,建模组和验证组中3条曲线走势基本相同(P>0.05),提示模型具有较好的预测价值,见图2C~D。
3 讨论
绝大多数的MIBC伴发于导管原位癌,术前穿刺难以诊断微浸润,往往是乳房病灶手术切除后才确诊,鉴于MIBC患者较少发生腋窝淋巴结转移,关于是否对MIBC患者行常规腋窝淋巴结手术评估一直以来争议不断。虽然前哨淋巴结活检是目前MIBC患者常用的腋窝淋巴结评估手段,较腋窝淋巴结清扫,已大大降低了手术并发症[8]。但前哨淋巴结活检依然是有创操作,依然有感觉异常、淋巴水肿、肩关节外展缺陷等手术风险[9-10]。本研究纳入的
6741 例MIBC患者中,发生ALNM的患者为309例,约占4.58%,与既往报道的转移率0~11%相当[11-12]。本研究还发现90%患者腋窝淋巴结转移为N1(278例),N2及N3患者约占10%(31例)。进一步说明了MIBC发生腋窝淋巴结转移的风险低,且腋窝转移的范围大部分较小。也说明常规对MIBC行腋窝淋巴结手术对大部分患者可能存在过度治疗。故评估MIBC患者ALNM风险,对MIBC患者腋窝淋巴结手术分期行个体化处理,可能将豁免部分患者的腋窝手术。既往研究表明,年龄是乳腺癌复发转移风险的影响因素,年轻乳腺癌具有更高的ALNM率及复发风险[13-14]。本研究发现≤40岁MIBC患者ALNM的风险约为41~60岁患者的2倍,是≥61岁患者的4~5倍。 乳腺癌组织学分级与ALNM风险相关[15],国外学者Parikh等探讨了SLNB在MIBC中的作用,认为对于较小的、组织学分级较低的肿瘤,可以考虑豁免SLNB[11]。在一项回顾性分析中, Hacking等也发现SLNB在更年轻、肿瘤较大、组织学分级较高的MIBC患者中应用更广泛[7]。另外在一项入组
2609 例MIBC患者的回顾性研究中,Fan等研究得出组织学分级较低的肿瘤与较低的前哨淋巴结转移率相关[4]。本研究也发现组织学分级Ⅱ、Ⅲ级的MIBC患者存在更高的ALNM风险。分子分型是乳腺癌重要的生物学特征之一,研究表明不同分子亚型乳腺癌ALNM风险有差异,但结论不一[16-18]。本研究通过多因素分析发现分子亚型与MIBC患者ALNM相关,通过列线图也发现三阴性亚型ALNM风险得分最高,但HR+HER2+、HR−HER2+、HR−HER2−三种分子亚型MIBC与HR+HER2−亚型间ALNM风险差异均无统计学意义,故本研究并不能得知哪种亚型MIBC患者ALNM风险最高。
多因素回归分析中我们还发现,不同种族MIBC患者ALNM风险有差异,黑种人腋窝淋巴结转移的风险是白种人的1.537倍。回顾既往研究也有类似结论,如宋文静等在构建年轻乳腺癌患者 ALNM的风险预测模型的研究中发现黑种人乳腺癌患者ALNM风险是白种人的约1.11倍[19]。Yip等在一项关于预测ALNM风险的研究中并未发现种族与ALNM相关,但该研究并未将种族按白种人、黑种人分组[20]。本研究多因素分析提示边侧是MIBC腋窝淋巴结转移风险的独立影响因素,但国内外关于边侧与乳腺癌腋窝淋巴结转移的相关性报道极少。根据列线图可知,边侧对风险总分的贡献较小。因此,边侧对MIBC腋窝淋巴结转移的影响可能需要更多的研究。
综上,本研究结果提示列线图具有较好的预测能力,有望在临床实践中对部分ALNM风险较小的MIBC患者豁免腋窝前哨淋巴结活检起到一定的参考作用。本研究为回顾性研究,数据主要来源于美国数据库,多为西方人群资料,而不同人种MIBC患者的临床病理特征可能有一定差异,故本研究构建的列线图预测模型对中国MIBC患者可能会存在一定偏倚。另外,SEER数据库中缺乏患者Ki-67信息,本研究在纳入变量时也存在一定的局限性。未来我们计划联合更多地区医疗中心,收集不同地区中国人群的数据,进一步验证并完善该模型,希望可以更好的服务于临床。
Competing interests: The authors declare that they have no competing interests.利益冲突声明:所有作者均声明不存在利益冲突。作者贡献:刘程浩:数据收集、统计分析、文章撰写及修改鲁 婷:统计分析、文章修改钱 芳:统计分析徐元兵:文章修改胡超华:研究指导沈浩元:提出研究思路与方案、参与文章修改及审校 -
表 1 微浸润乳腺癌患者临床病理资料[n(%)]
Table 1 Clinicopathological data of MIBC patients (n (%))
Characteristics Training
cohort
(n=4475)Validation
cohort
(n=2266)Total
(n=6741)Age(years) ≤40 270(6.03) 149(6.58) 419(6.22) 41-60 2364(52.83) 1066(47.04) 3430(50.88) 61-80 1684(37.63) 988(43.60) 2672(39.64) ≥81 157(3.51) 63(2.78) 220(3.26) Race White 3307(73.90) 1543(68.09) 4850(71.95) Black 517(11.55) 279(12.31) 796(11.81) Others/
Unknown651(14.55) 444(19.59) 1095(16.24) Grade Ⅰ 768(17.16) 399(17.61) 1167(17.31) Ⅱ 1223(27.33) 538(23.74) 1761(26.12) Ⅲ 867(19.37) 215(9.49) 1082(16.05) Ⅳ 44(0.98) 2(0.09) 46(0.68) Unknown 1573(35.15) 1112(49.07) 2685(39.83) Histologic type IDC 3919(87.58) 2043(90.16) 5962(88.44) Others 556(12.42) 223(9.84) 779(11.56) Subtype HR+HER2− 1604(35.84) 939(41.44) 2543(37.72) HR+HER2+ 503(11.24) 232(10.24) 735(10.90) HR−HER2+ 468(10.46) 235(10.37) 703(10.43) HR−HER2− 236(5.27) 110(4.85) 346(5.13) Unknown 1664(37.18) 750(33.10) 2414(35.81) Primary site
(quadrant of
breast)Upper-outer 1559(34.84) 755(33.32) 2314(34.33) Lower-outer 314(7.02) 199(8.78) 513(7.61) Upper-inner 471(10.53) 234(10.33) 705(10.46) Lower-inner 302(6.75) 147(6.49) 449(6.67) Central portion 226(5.05) 145(6.40) 371(5.50) Axillary tail 16(0.36) 6(0.26) 22(0.33) Overlapping
lesion949(21.21) 550(24.27) 1499(22.24) Nipple 14(0.31) 6(0.26) 20(0.30) Breast, NOS 624(13.94) 224(9.89) 848(12.58) Marital status Married 2723(60.85) 1405(62.00) 4128(61.24) Unmarried 1516(33.88) 760(33.54) 2276(33.76) Unknown 236(5.27) 101(4.46) 337(5.00) Laterality(origin
of primary)Left 2330(52.07) 1189(52.47) 3519(52.20) Right 2145(47.93) 1077(47.53) 3222(47.80) N N0 4250(94.97) 2182(96.29) 6432(95.42) N+ 225(5.03) 84(3.71) 309(4.58) Notes: MIBC: microinvasive breast cancer; Grade Ⅳ: undifferentiated; N: Ipsilateral axillary lymph nodes; N+: positive axillary lymph nodes; IDC: infiltrating duct carcinoma; Unmarried included single (never married), divorced, separated, widowed, domestic partner; NOS: not otherwise specified. 表 2 MIBC患者ALNM的单因素分析
Table 2 Univariate analysis of ALNM in MIBC patients
Characteristics N0 N+ χ2 or Fisher P Age(years) 57.386 <0.001 ≤40 236 34 41-60 2223 141 61-80 1639 45 ≥81 152 5 Race 10.118 0.006 White 3147 160 Black 477 40 Others/Unknown 626 25 Grade 38.198 <0.001 Ⅰ 748 20 Ⅱ 1160 63 Ⅲ 791 76 Ⅳ 43 1 Unknown 1508 65 Histologic type 5.162 0.023 IDC 3711 208 Others 539 17 Subtype 46.027 <0.001 HR+HER2− 1527 77 HR+HER2+ 459 44 HR−HER2+ 432 36 HR−HER2− 215 21 Unknown 1617 47 Primary Site
(quadrant of breast)12.588 0.109 Upper-outer 1485 74 Lower-outer 304 10 Upper-inner 453 18 Lower-inner 289 13 Central portion 214 12 Axillary tail 15 1 Overlapping lesion 900 49 Nipple 13 1 Breast, NOS 577 47 Marital status 4.703 0.095 Married 2596 127 Unmarried 1426 90 Unknown 228 8 Laterality
(origin of primary)6.877 0.009 Left 2232 98 Right 2018 127 Note: ALNM: axillary lymph node metastasis. 表 3 MIBC患者ALNM的多因素Logistic回归分析
Table 3 Multivariate Logistic regression analysis of ALNM in MIBC patients
Characteristics OR 95%CI P Age(years) <0.001 ≤40 1 41-60 0.460 0.306-0.692 <0.001 61-80 0.214 0.132-0.346 <0.001 ≥81 0.251 0.095-0.665 <0.001 Race 0.014 White 1 Black 1.537 1.061-2.226 0.023 Others/Unknown 0.727 0.469-1.125 0.152 Grade <0.001 Ⅰ 1 Ⅱ 1.720 1.019-2.905 0.042 Ⅲ 2.917 1.707-4.985 <0.001 Ⅳ 0.830 0.106-6.491 0.859 Unknown 1.533 0.901-2.606 0.115 Subtype <0.001 HR+HER2− 1 HR+HER2+ 1.329 0.887-1.992 0.168 HR−HER2+ 1.082 0.696-1.681 0.726 HR−HER2− 1.493 0.882-2.528 0.136 Unknown 0.477 0.324-0.700 <0.001 Laterality(origin of primary) 0.013 Left 1 Right 1.420 1.077-1.871 0.013 -
[1] SungH, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries[J]. CA A Cancer J Clin, 2021, 71(3): 209-249. doi: 10.3322/caac.21660
[2] de Mascarel I, MacGrogan G, Mathoulin-Pélissier S, et al. Breast ductal carcinoma in situ with microinvasion[J]. Cancer, 2002, 94(8): 2134-2142. doi: 10.1002/cncr.10451
[3] Xu H, Han Y, Wu Y, et al. Clinicopathological characteristics and prognosis of microinvasive breast cancer: A population-based analysis[J]. Cancer Med, 2022, 11(23): 4501-4512. doi: 10.1002/cam4.4839
[4] Fan B, Pardo JA, Serres S, et al. Role of Sentinel Lymph Node Biopsy in Microinvasive Breast Cancer[J]. Ann Surg Oncol, 2020, 27(11): 4468-4473. doi: 10.1245/s10434-020-08606-3
[5] Gojon H, Fawunmi D, Valachis A. Sentinel lymph node biopsy in patients with microinvasive breast cancer: A systematic review and meta-analysis[J]. Eur J Surg Oncol, 2014, 40(1): 5-11. doi: 10.1016/j.ejso.2013.10.020
[6] James TA, Fan B. ASO Author Reflections: Limiting Axillary Surgery for Microinvasive Breast Cancer[J]. Ann Surg Oncol, 2020, 27(11): 4474. doi: 10.1245/s10434-020-08694-1
[7] Hacking SM, Leonard KL, Wu D, et al. Microinvasive breast cancer and the role of sentinel lymph node biopsy[J]. Sci Rep, 2022, 12(1): 12391. doi: 10.1038/s41598-022-16521-8
[8] Sun SX, Moseley TW, Kuerer HM, et al. Imaging-Based Approach to Axillary Lymph Node Staging and Sentinel Lymph Node Biopsy in Patients With Breast Cancer[J]. Am J Roentgenol, 2020, 214(2): 249-258. doi: 10.2214/AJR.19.22022
[9] Ashikaga T, Krag DN, Land SR, et al. Morbidity results from the NSABP B-32 trial comparing sentinel lymph node dissection versus axillary dissection[J]. J Surg Oncol, 2010, 102(2): 111-118. doi: 10.1002/jso.21535
[10] Che Bakri NA, Kwasnicki RM, Khan N, et al. Impact of Axillary Lymph Node Dissection and Sentinel Lymph Node Biopsy on Upper Limb Morbidity in Breast Cancer Patients[J]. Ann Surg, 2023, 277(4): 572-580. doi: 10.1097/SLA.0000000000005671
[11] Parikh RR, Haffty BG, Lannin D, et al. Ductal Carcinoma In Situ With Microinvasion: Prognostic Implications, Long-Term Outcomes, and Role of Axillary Evaluation[J]. Int J Radiat Oncol Biol Phys, 2012, 82(1): 7-13. doi: 10.1016/j.ijrobp.2010.08.027
[12] Magnoni F, Massari G, Santomauro G, et al. Sentinel lymph node biopsy in microinvasive ductal carcinomain situ[J]. Br J Surg, 2019, 106(4): 375-383. doi: 10.1002/bjs.11079
[13] Azim HA, Partridge AH. Biology of breast cancer in young women[J]. Breast Cancer Res, 2014, 16(4): 427. doi: 10.1186/s13058-014-0427-5
[14] Paluch-Shimon S, Cardoso F, Partridge AH, et al. ESO-ESMO fifth international consensus guidelines for breast cancer in young women (BCY5)[J]. Ann Oncol, 2022, 33(11): 1097-1118. doi: 10.1016/j.annonc.2022.07.007
[15] Gao X, Luo W, He L, et al. Nomogram models for stratified prediction of axillary lymph node metastasis in breast cancer patients (cN0)[J]. Front Endocrinol (Lausanne), 2022, 13: 967062. doi: 10.3389/fendo.2022.967062
[16] Xiong J, Zuo W, Wu Y, et al. Ultrasonography and clinicopathological features of breast cancer in predicting axillary lymph node metastases[J]. BMC Cancer, 2022, 22(1): 1155. doi: 10.1186/s12885-022-10240-z
[17] Pereira A, Siegrist J, Lizarraga S, et al. Clustering Molecular Subtypes in Breast Cancer, Immunohistochemical Parameters and Risk of Axillary Nodal Involvement[J]. J Pers Med, 2022, 12(9): 1404. doi: 10.3390/jpm12091404
[18] Dihge L, Bendahl PO, Rydén L. Nomograms for preoperative prediction of axillary nodal status in breast cancer[J]. Br J Surg, 2017, 104(11): 1494-1505. doi: 10.1002/bjs.10583
[19] 宋文静, 贺鑫, 龚鹏举, 等. 基于临床病理大数据的早发乳腺癌腋窝淋巴结转移风险预测模型构建[J]. 中国普通外科杂志, 2020, 29(11): 1293-1302. [Song WJ, He X, Gong PJ, et al. Establishment of risk prediction model for axillary lymph node metastasis in breast cancer at early age based on clinicopathologic big data[J]. Zhongguo Pu Tong Wai Ke Za Zhi, 2020, 29(11): 1293-1302.] doi: 10.7659/j.issn.1005-6947.2020.11.002 Song WJ, He X, Gong PJ, et al. Establishment of risk prediction model for axillary lymph node metastasis in breast cancer at early age based on clinicopathologic big data[J]. Zhongguo Pu Tong Wai Ke Za Zhi, 2020, 29(11): 1293-1302. doi: 10.7659/j.issn.1005-6947.2020.11.002
[20] Yip CH, Taib NA, Tan GH, et al. Predictors of Axillary Lymph Node Metastases in Breast Cancer: Is There a Role for Minimal Axillary Surgery?[J]. World J Surg, 2009, 33(1): 54-57. doi: 10.1007/s00268-008-9782-7



 下载:
下载: