Role of Preoperative Peripheral Blood Inflammatory Parameters and Postoperative Lymph-node Ratio in Prognosis of Patients with Gastric Cancer Undergoing Chemotherapy
-
摘要:目的
分析术前外周血炎性参数与术后淋巴结比率(LNR)在胃癌化疗患者预后中的作用。
方法按外周血中性粒细胞与淋巴细胞比率(NLR)、血小板-淋巴细胞比率(PLR)、全身免疫炎性反应指数(SII)、淋巴细胞-单核细胞比率(LMR)、小野寺预后营养指数(OPNI)、LNR截断值将108例胃癌患者分为高低两组,分析这些炎性参数对胃癌化疗患者总生存期(OS)的预后价值。以独立预后指标绘制列线图预测胃癌患者的存活率。
结果NLR在胃癌化疗患者的预后评估中有统计学意义(P < 0.001),高PLR组、高SII组、高LNR组、N3分期、TNM(Ⅲ~Ⅳ)分期、神经侵犯、癌胚抗原(CEA)是胃癌预后的独立危险因素(均P < 0.05)。LNR、PLR及SII三者组合(AUC=0.875)在胃癌预后方面的预测效果优于单独或两两联合。
结论NLR、LNR、PLR及SII升高与患者的生存期显著减少相关;LNR、PLR及SII可作为胃癌化疗患者预后的独立危险因素,三者联合可预测胃癌患者的生存期。
Abstract:ObjectiveTo analyze the role of preoperative peripheral blood inflammatory parameters and postoperative lymph-node ratio (LNR) in the prognosis of gastric cancer patients treated with chemotherapy.
MethodsThe neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), systemic immune inflammatory response index (SII), lymphocyte-to-monocyte ratio (LMR), Onodera prognostic nutritional index (OPNI), and LNR of 108 patients with gastric cancer were classified into high and low groups to analyze their prognostic value on the overall survival (OS) of gastric cancer patients treated with chemotherapy. The independent prognostic indicators were plotted in columns to predict the survival rate of gastric cancer patients.
ResultsNLR was statistically significant in the prognostic assessment of gastric cancer patients treated with chemotherapy (P < 0.001). Moreover, the high PLR group, high SII group, high LNR group, N3 stage, TNM (Ⅲ-Ⅳ) stage, nerve invasion, and carcinoembryonic antigen (CEA) were independent risk factors for the prognosis of gastric cancer (all P < 0.05). These findings indicated that in predicting the prognosis of gastric cancer, the combination of LNR, PLR, and SII (AUC=0.875) was better than that of LNR, PLR, and SII alone or in pairwise combination.
ConclusionElevated NLR, LNR, PLR, and SII are associated with significantly reduced survival of patients. LNR, PLR, and SII could be used as independent risk factors for the prognosis of gastric cancer patients treated with chemotherapy, and their combination can predict the survival of gastric cancer patients.
-
Key words:
- LNR /
- Peripheral blood inflammatory parameters /
- Gastric cancer /
- Prognosis
-
0 引言
胃癌是全球癌症相关死亡的第三大原因,早期胃癌患者的5年总生存率可达90%以上,而晚期胃癌患者5年生存率低于15%[1-2]。因此,探寻有效的肿瘤诊断标志物及治疗方法尤为重要。
研究发现外周血炎性反应参数与肿瘤进展之间存在密切关系[3-5]。以中性粒细胞与淋巴细胞比率(neutrophil-to-lymphocyte ratio, NLR)、血小板-淋巴细胞比率(platelet-to-lymphocyte ratio, PLR)为代表的炎性反应参数与包括胃癌在内的多种癌症的诊断和预后密切相关[6-8]。随着对外周血的深入探究,其他炎性参数如SII被证明与多种癌症预后相关[9]。以炎性反应参数为基础的多种联合指标在预测癌症的生存期中被拓展。Cheng[10]和Liu[11]团队分别证实三级淋巴结构(TLS)和纤维蛋白原(F)联合NLR在肿瘤预后中意义重大。当前,关于术前炎性参数与胃癌患者预后价值间的关系仍有待进一步探索。此外,对肿瘤患者而言,更精准的治疗方案及预后评估举足轻重。研究者们发现,淋巴结转移作为胃癌转移的主要途径,其术后淋巴结状态对胃癌患者的预后评估至关重要。有学者[12-13]提出淋巴结比率(lymph-node ratio, LNR)分期较现有的病理N分期能更好地评估胃癌术后患者的预后情况。LNR分期可以极大限度地降低由于获取的淋巴结数量不足导致的阶段迁移现象,是研究者们证实最有可能代替或辅助现有术后N分期的新型淋巴结分期[14]。本文就术前炎性反应相关参数、术后LNR分期在胃癌化疗患者预后中的作用进行相关性分析。
1 资料与方法
1.1 一般资料及分组
回顾性纳入2016年1月至2020年12月恩施土家族苗族自治州中心医院胃肠外科收治的胃癌患者资料并随访至2021年12月。纳入标准:(1)经穿刺活检、临床、影像学检查且术后病检明确诊断为胃癌患者;(2)病例资料及回访资料完整;(3)术后予以辅助化疗。排除标准:(1)合并严重糖尿病、心力衰竭、肝和(或)肾功能衰竭;(2)有精神疾病及不配合者;(3)合并其他恶性肿瘤病史;(4)围手术期行新辅助治疗。最终纳入108例胃癌患者。本研究经恩施州中心医院伦理委员会批准。通过医院病历系统获取患者的临床信息,研究通过了医院审批,患者免知情。
1.2 研究方法
所有患者术后常规化疗,每三周复查一次直至第6或第8疗程结束,每6个月至1年复查一次,通过电话随访获取患者生存状态。从电子病历中获取患者的年龄、性别、肿瘤直径、肿瘤发生部位、分化程度、与周围侵犯关系、手术获取的阳性淋巴结数目及其总数、术前外周血细胞计数。其中,计数资料包括NLR、PLR、淋巴细胞-单核细胞比率(lymphocyte-to-monocyte ratio, LMR)、小野寺预后营养指数(onodera prognostic nutritional index, OPNI)(OPNI=血清白蛋白+5×总淋巴细胞计数)和SII(SII=血小板计数×中性粒细胞计数/淋巴细胞计数)在内的全身炎性参数。总生存期(OS)定义为从疾病确诊到死亡或随访截止时间。
1.3 统计学方法
使用R version4.2.1和SPSS23.00进行统计分析。计数资料以频数、率表示,计量资料以均数±标准差显示,组间比较采用卡方检验;使用R软件survminer包来确定LNR、PLR、SII、NLR、OPIN、LMR、年龄、肿瘤直径大小的截断值。通过Cox比例风险回归分析来确定与OS相关的参数。P < 0.05为差异有统计学意义。
2 结果
2.1 患者临床特征
本研究回顾性招募了108例根治性胃癌术后患者。其中,男66例,女42例,年龄32~76岁,中位年龄55岁,平均年龄54.83±19.83岁。胃上部肿瘤有83例、胃中部肿瘤17例、胃下部肿瘤6例、全胃肿瘤有2例。此外,中-高分化胃癌29例,低-未分化胃癌79例。根据AJCC第八版术后病理分期,处于Ⅰ~Ⅱ期胃癌54例,Ⅲ~Ⅳ期54例。
2.2 临床相关基线、外周血炎性反应指标截断值的制定及预后价值
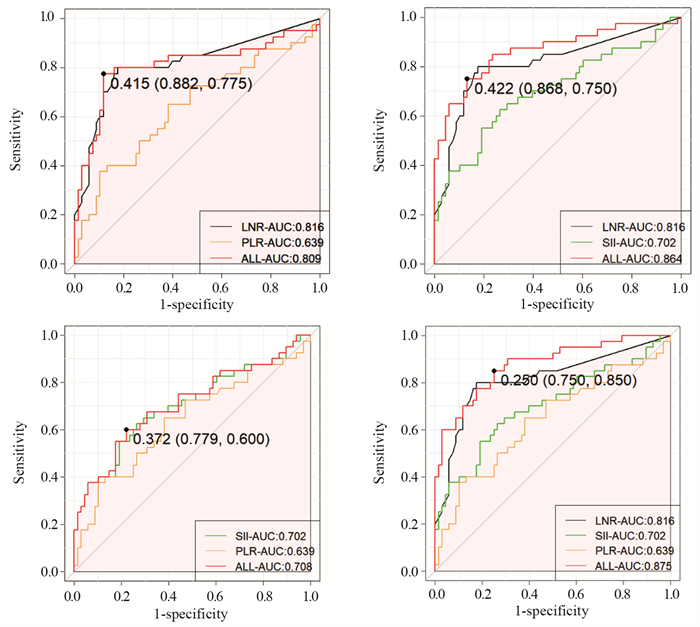
通过R软件来确定每个参数的最佳截止值。按年龄、肿瘤大小、LNR、PLR、SII、NLR、OPIN、LMR截断值将患者分为两组。统计发现高年龄组(≥52岁)、肿瘤大直径组(≥3 cm)、高LNR组(≥0.29)、高PLR组(≥195.54)、高SII组(≥795.05)、高NLR组(≥2.25)以及低OPIN组(≤40.99)的中位生存期分别为60.3、53.9、24.5、29.9、29.9、36.3和46.7个月。同时通过两两联合发现高LNR+PLR联合组及高PLR+SII联合组中位生存时间均为22.6个月,而LMR组及其他对应组别患者死亡率均小于50%。在胃癌患者预后预测方面,LNR的ROC曲线下面积(AUC)达到0.816,相较于炎性参数SII、NLR、PLR、LMR、肿瘤大小及淋巴结分期有更好的生存预测价值,见图 1。
2.3 外周血炎性参数、淋巴结比率与胃癌临床特征之间的相关性
结果显示,LNR与肿瘤侵犯浆膜层、神经、血管、TNM分期,淋巴结转移及肿瘤大小相关(P < 0.05)。SII仅与肿瘤TNM分期相关;PLR与肿瘤侵犯浆膜层、神经、血管、TNM分期、淋巴结转移、肿瘤大小及肿瘤标志物CEA和CA125相关(P < 0.05)。NLR与肿瘤侵犯神经、血管、淋巴结分期、M分期及CEA相关;LMR与年龄、肿瘤侵犯浆膜、T分期、肿瘤TNM分期、淋巴结转移及CEA相关;OPNI与肿瘤侵犯浆膜层、淋巴结分期、TNM分期及CA125相关(P < 0.05),见表 1~2。
表 1 LNR、SII、PLR与胃癌临床特征相关分析(n(%))Table 1 Correlation of LNR, SII, and PLR with clinical features of gastric cancer patients (n(%)) 表 2 NLR、LMR、OPNI与胃癌临床特征相关分析(n(%))Table 2 Correlation of NLR, LMR, and OPNI with clinical features of gastric cancer patients (n(%))
表 2 NLR、LMR、OPNI与胃癌临床特征相关分析(n(%))Table 2 Correlation of NLR, LMR, and OPNI with clinical features of gastric cancer patients (n(%))
2.4 胃癌患者预后影响因素分析
根据Cox单因素回归分析显示侵犯浆膜层、侵犯神经及血管、T分期、N分期、M分期、TNM分期、肿瘤大小、肿瘤发生于全胃、淋巴结转移、LNR、PLR、SII、NLR、CEA、CA125是胃癌患者预后影响因素(P < 0.05);Cox多因素分析表明侵犯神经、N3分期、胃癌Ⅲ~Ⅳ期、高LNR分期、高SII、高PLR、CEA是胃癌OS的独立风险因素(P < 0.05),见表 3。
表 3 胃癌总生存期影响因素的Cox单因素和多因素分析Table 3 Cox univariate and multivariate analyses of influencing factors for overall survival of gastric cancer patients
2.5 LNR、PLR、SII组合与胃癌预后的关系
通过ROC曲线下面积来预测胃癌患者的预后价值。结果显示单独LNR、PLR和SII的AUC分别为0.816、0.639和0.702;LNR与SII组合(AUC:0.864,敏感度:86.8%,特异度:75%)及LNR与PLR组合(AUC:0.816,敏感度:88.2%,特异度:77.5%)能较好地预测胃癌OS,而SII与PLR组合(AUC:0.708,敏感度:77.9%,特异度:60%)略差,并发现当LNR、SII和PLR三者组合时AUC最大达0.875,预测价值最大,见图 1。
2.6 构建列线图提供可靠的生存预测
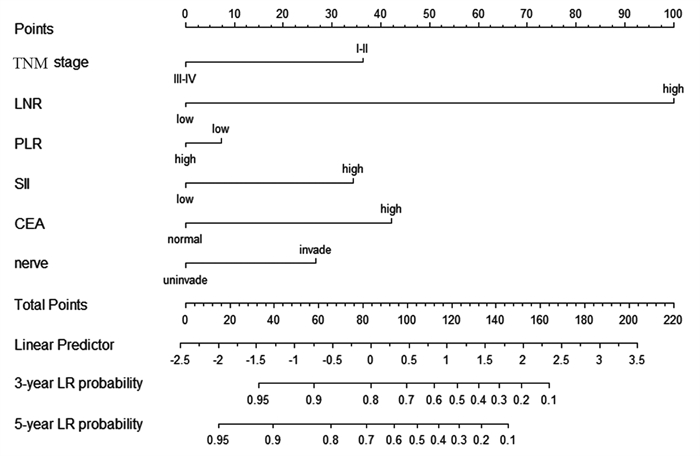
基于多变量Cox回归分析中确定的预测因子构建列线图以预测生存率。该列线图主要基于LNR、PLR、TNM分期、SII、CEA、神经受累开发的,用来预测3年和5年的OS概率。为每个因素水平分配一个积分量表分数,并将因素分数相加以获得总分,例如LNR分期(70分),PLR(5分),TNM分期(20分),SII(10分),CEA(20分),神经受累(15分),总得分为140分,在这种条件下,患者的3年和5年生存率分别为32%和15%,见图 2。
3 讨论
近年来,学者们发现癌症的进展不仅取决于肿瘤的特征,还取决于宿主的免疫及炎性反应,癌症相关炎性反应可以通过抑制抗肿瘤免疫而促进肿瘤的发展及转移[15-16]。研究[17-22]证实炎性反应因子与恶性肿瘤的发生发展密切相关,促进了恶性肿瘤的侵袭和转移。如在慢性病毒性肝炎发展为肝硬化进而导致肝癌和长期的慢性胃炎进展为胃癌中,炎性因子在促进癌细胞增殖、血管化和转移中起重要作用[23-24]。
临床上,术前外周血炎性反应指标参数获取简便。尤其在肿瘤预后方面,以炎性参数为基点寻找有效的预后标志物不仅能为患者提供更精准的规范化治疗,同时也为患者减轻不必要的经济负担。2001年,Zahorec团队在研究中观察到癌症患者淋巴细胞减少的同时伴随着持续中性粒细胞增多后,首次提出将NLR作为炎性反应标志物[25]。自此,围绕NLR为中心的各项研究就此展开。一方面,中性粒细胞可以通过抑制NK细胞、淋巴细胞和活化的T细胞的活性来抑制免疫系统[26-27];另一方面,中性粒细胞可以通过产生血管内皮生长因子来促进肿瘤的血管生成和进展[28]。因此,以NLR为首的炎性参数研究报道相继在胃癌,结直肠癌、肝癌、乳腺癌等癌症中被证实与预后相关[29]。在胃癌方面,Fang等[30]发现NLR和PLR对早期胃癌的诊断价值高于传统的肿瘤标志物CEA和CA19-9,为早期胃癌的筛查提供了参考价值。随后Wang[31]和陈奕心[32]等先后证实以NLR为代表的炎性反应参数在胃癌预后中的作用。而Mungan等[33]的研究结果表明术前PLR与胃癌的死亡率相关,NLR则对胃癌复发的预测更为敏感。为了更进一步证明炎性反应相关参数在胃癌中的价值,本研究纳入了近年来研究的热点炎性反应参数来研究其在胃癌化疗中的预后价值,结果发现高NLR、PLR及SII与胃癌化疗患者生存期显著缩短相关,其中PLR及SII可以作为胃癌化疗患者生存期的独立预后因素,而NLR并非其独立预后因子,这一结果与Miyamoto等[34]研究存在差异,可能是样本量不足所致。此外,本研究发现LMR、OPNI相关炎性反应参数在评估胃癌患者化疗的总生存期方面无显著意义。
为了更精准地评估患者预后,本研究引入了LNR分期(新N分期)。当前,临床上以胃癌根治术为中心的多学科综合治疗成为攻克胃癌的主要方式。其中,淋巴结转移是胃癌转移的主要途径,而术后淋巴结状态对胃癌患者的预后评估至关重要。精准的淋巴结分期不仅能为患者提供更个性化的治疗,同时能进一步评估患者治疗后状态。LNR分期已被多位学者证实在胃癌中的作用。Wang等[35]通过对18 000例胃癌患者的预后进行分析表明:使用LNR分期的偏倚(12%)明显低于TNM分期的偏倚(57%)。Liu等[36]则通过对18年的数据分析发现,LNR分期在获取LN > 25个的所有淋巴结阶段(从N1到N3b)的OS更具优势。因此本研究将术后LNR分期与术前外周血相关参数结合,发现当高LNR分期组与高SII组联合时胃癌患者中位生存期最低达18.1个月,而将LNR、PLR、SII三者联合时并未得到理想结果。同时通过相关性分析发现LNR与NLR、PLR、SII关联不大(r < 0.3)。但在胃癌化疗患者的预后评估方面,LNR、PLR及SII三者组合效果最好,为临床上胃癌患者的诊疗提供了重要参考。本研究不足之处在于非大样本实验;同时LNR分期是部分学者认为可能替代或辅助肿瘤分期的新N分期,后期还需大量研究证实。此外,炎性相关参数及LNR分期截断值的多样性也限制了其在临床上的应用,后期仍需进一步探索。
总的来说,本研究引入了部分炎性参数并证实了外周血相关参数及LNR分期在可行手术并予以术后辅助化疗的胃癌中的预后价值,并首次联合评估了其对胃癌患者的预后价值,为胃癌临床应用及基础研究提供了新思路。同时设计的列线图可以更容易地帮助临床医生评估胃癌患者的预后,以便后期制定更加精准和个体化的诊疗方案。
Competing interests: The authors declare that they have no competing interests.利益冲突声明:所有作者均声明不存在利益冲突。作者贡献:任文镇:研究设计、资料收集、统计分析、论文撰写王宏浩:文献查阅、统计分析向 田:资料收集、文献查阅刘 杲:研究设计、论文审阅、论文修改 -
表 1 LNR、SII、PLR与胃癌临床特征相关分析(n(%))
Table 1 Correlation of LNR, SII, and PLR with clinical features of gastric cancer patients (n(%))

表 2 NLR、LMR、OPNI与胃癌临床特征相关分析(n(%))
Table 2 Correlation of NLR, LMR, and OPNI with clinical features of gastric cancer patients (n(%))

表 3 胃癌总生存期影响因素的Cox单因素和多因素分析
Table 3 Cox univariate and multivariate analyses of influencing factors for overall survival of gastric cancer patients

-
[1] Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries[J]. CA Cancer J Clin, 2021, 71(3): 209-249. doi: 10.3322/caac.21660
[2] Li P, Chen H, Chen S, et al. Circular RNA 0000096 affects cell growth and migration in gastric cancer[J]. Br J Cancer, 2017, 116(5): 626-633. doi: 10.1038/bjc.2016.451
[3] Mollinedo F. Neutrophil Degranulation, Plasticity, and Cancer Metastasis[J]. Trends Immunol, 2019, 40(3): 228-242. doi: 10.1016/j.it.2019.01.006
[4] Xiong S, Dong L, Cheng L. Neutrophils in cancer carcinogenesis and metastasis[J]. J Hematol Oncol, 2021, 14(1): 173. doi: 10.1186/s13045-021-01187-y
[5] Zare Moayedi M, Ahmmadpour F, Rashidi M, et al. The association between mRNA expression of resistin, TNF-α, IL-6, IL-8, and ER-α in peripheral blood mononuclear cells and breast cancer[J]. Turk J Med Sci, 2021, 51(3): 1345-1353. doi: 10.3906/sag-2008-292
[6] Hirahara T, Arigami T, Yanagita S, et al. Combined neutrophil-lymphocyte ratio and platelet-lymphocyte ratio predicts chemotherapy response and prognosis in patients with advanced gastric cancer[J]. BMC cancer, 2019, 19(1): 672. doi: 10.1186/s12885-019-5903-y
[7] Trinh H, Dzul S P, Hyder J, et al. Prognostic value of changes in neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR) and lymphocyte-to-monocyte ratio (LMR) for patients with cervical cancer undergoing definitive chemoradiotherapy (dCRT)[J]. Clin Chim Acta, 2020, 510: 711-716. doi: 10.1016/j.cca.2020.09.008
[8] Xia LJ, Li W, Zhai JC, et al. Significance of neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, lymphocyte-to-monocyte ratio and prognostic nutritional index for predicting clinical outcomes in T1-2 rectal cancer[J]. BMC cancer, 2020, 20(1): 208. doi: 10.1186/s12885-020-6698-6
[9] Huang Y, Gao Y, Wu Y, et al. Prognostic value of systemic immune-inflammation index in patients with urologic cancers: a meta-analysis[J]. Cancer Cell Int, 2020, 20: 499. doi: 10.1186/s12935-020-01590-4
[10] Cheng H, Luo G, Lu Y, et al. The combination of systemic inflammation-based marker NLR and circulating regulatory T cells predicts the prognosis of resectable pancreatic cancer patients[J]. Pancreatology, 2016, 16(6): 1080-1084. doi: 10.1016/j.pan.2016.09.007
[11] Liu R, Dai T, Zheng S, et al. Prognostic value of combined pretreatment fibrinogen and neutrophil-lymphocyte ratio in digestive system cancers: a meta-analysis of 17 retrospective studies[J]. Transl Cancer Res, 2021, 10(1): 241-250. doi: 10.21037/tcr-20-2482
[12] Huang Z, Chen Y, Zhang W, et al. Modified Gastric Cancer AJCC Staging with a Classification Based on the Ratio of Regional Lymph Node Involvement: A Population-Based Cohort Study[J]. Ann Surg Oncol, 2020, 27(5): 1480-1487. doi: 10.1245/s10434-019-08098-w
[13] Agnes A, Biondi A, Cananzi FM, et al. Ratio-based staging systems are better than the 7th and 8th editions of the TNM in stratifying the prognosis of gastric cancer patients: A multicenter retrospective study[J]. J Surg Oncol, 2019, 119(7): 948-957. doi: 10.1002/jso.25411
[14] Sakin A, Atci MM, Aldemir MN, et al. The Prognostic Value of Postoperative Lymph Node Ratio in Gastric Adenocarcinoma Patients Treated With Neoadjuvant Chemotherapy[J]. Cureus, 2021, 13(4): e14639. http://pubmed.ncbi.nlm.nih.gov/34046274/
[15] Stoltzfus CR, Sivakumar R, Kunz L, et al. Multi-Parameter Quantitative Imaging of Tumor Microenvironments Reveals Perivascular Immune Niches Associated With Anti-Tumor Immunity[J]. Front Immunol, 2021, 12: 726492. doi: 10.3389/fimmu.2021.726492
[16] Singh A, Anang V, Kumari K, et al. Role of lymphocytes, macrophages and immune receptors in suppression of tumor immunity[J]. Prog Mol Biol Transl Sci, 2023, 194: 269-310.
[17] Yu K, Qiang G, Peng S, et al. Potential diagnostic value of the hematological parameters lymphocyte-monocyte ratio and hemoglobin-platelet ratio for detecting colon cancer[J]. J Int Med Res, 2022, 50(9): 3000605221122742.
[18] Hajizadeh F, Aghebati Maleki L, Alexander M, et al. Tumor-associated neutrophils as new players in immunosuppressive process of the tumor microenvironment in breast cancer[J]. Life Sci, 2021, 264: 118699. doi: 10.1016/j.lfs.2020.118699
[19] Wang H, Zhang B, Li R, et al. KIAA1199 drives immune suppression to promote colorectal cancer liver metastasis by modulating neutrophil infiltration[J]. Hepatology, 2022, 76(4): 967-981. doi: 10.1002/hep.32383
[20] Huang Y, Chen Y, Zhu Y, et al. Postoperative Systemic Immune-Inflammation Index (SⅡ): A Superior Prognostic Factor of Endometrial Cancer[J]. Front Surg, 2021, 8: 704235. doi: 10.3389/fsurg.2021.704235
[21] Zahorec R. Neutrophil-to-lymphocyte ratio, past, present and future perspectives[J]. Bratisl Lek Listy, 2021, 122(7): 474-488.
[22] Jiang Y, Xu D, Song H, et al. Inflammation and nutrition-based biomarkers in the prognosis of oesophageal cancer: a systematic review and meta-analysis[J]. BMJ Open, 2021, 11(9): e048324. doi: 10.1136/bmjopen-2020-048324
[23] Swierczak A, Mouchemore KA, Hamilton JA, et al. Neutrophils: important contributors to tumor progression and metastasis[J]. Cancer Metastasis Rev, 2015, 34(4): 735-751. doi: 10.1007/s10555-015-9594-9
[24] Liang W, Ferrara N. The Complex Role of Neutrophils in Tumor Angiogenesis and Metastasis[J]. Cancer Immunol Res, 2016, 4(2): 83-91. doi: 10.1158/2326-6066.CIR-15-0313
[25] Zahorec R. Ratio of neutrophil to lymphocyte counts-rapid and simple parameter of systemic inflammation and stress in critically ill[J]. Bratisl Lek Listy, 2001, 102(1): 5-14. http://bmj.fmed.uniba.sk/2001/10201-01.PDF
[26] el-Hag A, Clark RA. Immunosuppression by activated human neutrophils. Dependence on the myeloperoxidase system[J]. J Immunol, 1987, 139(7): 2406-2413. doi: 10.4049/jimmunol.139.7.2406
[27] Petrie HT, Klassen LW, Kay HD. Inhibition of human cytotoxic T lymphocyte activity in vitro by autologous peripheral blood granulocytes[J]. J Immunol, 1985, 134(1): 230-234. doi: 10.4049/jimmunol.134.1.230
[28] Tan KW, Chong SZ, Wong FHS, et al. Neutrophils contribute to inflammatory lymphangiogenesis by increasing VEGF-A bioavailability and secreting VEGF-D[J]. Blood, 2013, 122(22): 3666-3677. doi: 10.1182/blood-2012-11-466532
[29] Templeton AJ, McNamara MG, Šeruga B, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis[J]. J Natl Cancer Inst, 2014, 106(6): dju124. http://jnci.oxfordjournals.org/content/106/6/dju124.full.pdf
[30] Fang T, Wang Y, Yin X, et al. Diagnostic Sensitivity of NLR and PLR in Early Diagnosis of Gastric Cancer[J]. J Immunol Res, 2020, 2020: 9146042. http://www.xueshufan.com/publication/3009855148
[31] Wang H, Ding Y, Li N, et al. Prognostic Value of Neutrophil-Lymphocyte Ratio, Platelet-Lymphocyte Ratio, and Combined Neutrophil-Lymphocyte Ratio and Platelet-Lymphocyte Ratio in Stage Ⅳ Advanced Gastric Cancer[J]. Front Oncol, 2020, 10: 841. doi: 10.3389/fonc.2020.00841
[32] 陈奕心, 孙轶华, 程洋洋, 等. 术前炎症相关指标与可切除胃癌患者预后的相关[J]. 实用肿瘤学杂志, 2021, 35(6): 517-522. https://www.cnki.com.cn/Article/CJFDTOTAL-SYZL202106008.htm Chen YX, Sun YH, Cheng YY, et al. Relationship between preoperative inflammation-related indicators and prognosis of patients with resectable gastric cancer[J]. Shi Yong Zhong Liu Xue Za Zhi, 2021, 35(6): 517-522. https://www.cnki.com.cn/Article/CJFDTOTAL-SYZL202106008.htm
[33] Mungan İ, Dicle Ç B, Bektaş Ş, et al. Does the preoperative platelet-to-lymphocyte ratio and neutrophil-to-lymphocyte ratio predict morbidity after gastrectomy for gastric cancer?[J]. Mil Med Res, 2020, 7: 9. http://www.xueshufan.com/publication/3018592043
[34] Miyamoto R, Inagawa S, Sano N, et al. The neutrophil-to-lymphocyte ratio (NLR) predicts short-term and long-term outcomes in gastric cancer patients[J]. Eur J Surg Oncol, 2018, 44(5): 607-612. doi: 10.1016/j.ejso.2018.02.003
[35] Wang J, Dang P, Raut CP, et al. Comparison of a lymph node ratio-based staging system with the 7th AJCC system for gastric cancer: analysis of 18, 043 patients from the SEER database[J]. Ann Surg, 2012, 255(3): 478-485. doi: 10.1097/SLA.0b013e31824857e2
[36] Liu YY, Fang WL, Wang F, et al. Does a Higher Cutoff Value of Lymph Node Retrieval Substantially Improve Survival in Patients With Advanced Gastric Cancer?-Time to Embrace a New Digit[J]. Oncologist, 2017, 22(1): 97-106. doi: 10.1634/theoncologist.2016-0239
-
期刊类型引用(2)
1. 陈慧娟, 施宝美, 邢利. 淋巴结比率联合AFP、CA199、CA724对宫颈癌手术患者的预后评估价值. 中华内分泌外科杂志. 2025(03)  百度学术
百度学术
2. 程龙龙,张诗涵,孟鑫,张静睿,周莹,王永功. 术前外周血炎症指标评价OSCC患者预后的研究进展. 中外医学研究. 2024(22): 180-184 .  百度学术
百度学术
其他类型引用(1)



 下载:
下载: