Clinical Prediction of Lung Cancer Complicated with Pulmonary Infection After Thoracoscopic Surgery Based on Nomogram Model
-
摘要:目的
分析肺癌患者胸腔镜根治术后并发肺部感染的危险因素并建立预测列线图模型。
方法选取2018年1月至2021年10月接受胸腔镜根治术的315例原发性肺癌患者作为研究对象,据患者术后是否发生肺部感染分为肺部感染组和非肺部感染组。收集两组临床资料进行单因素和回归分析,得出独立预测因素,基于此构建列线图风险模型并对该模型进行预测效能评价。
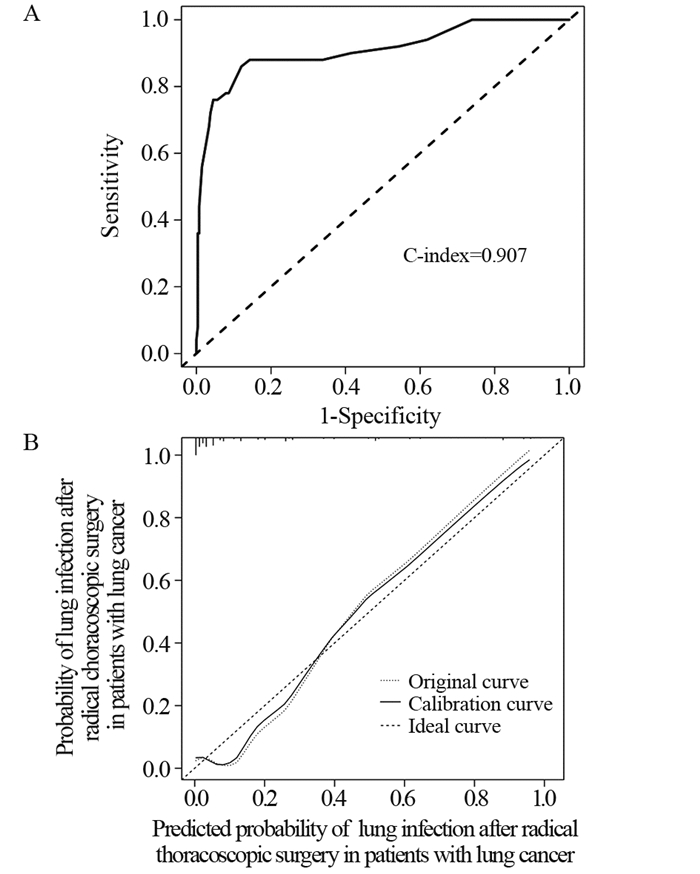
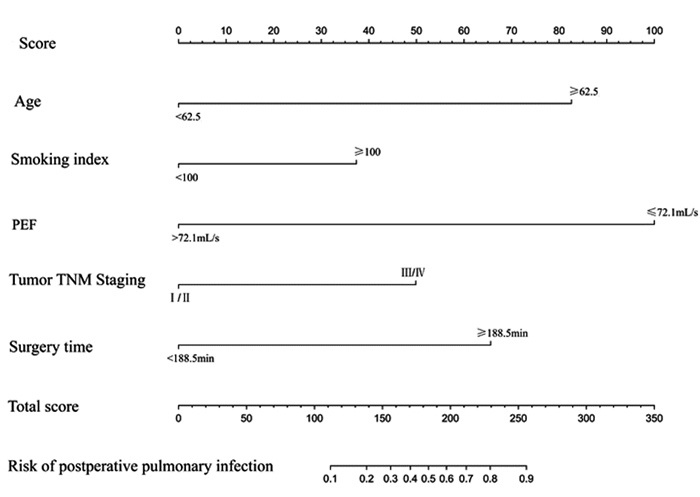
结果患者年龄≥62.5岁、吸烟指数≥100、PEF≤72.1 ml/s、TNM分期为Ⅲ/Ⅳ期和手术时间≥188.5 min是肺癌患者胸腔镜根治术后并发肺部感染的独立危险因素(P < 0.05)。基于以上影响因素建立列线图风险模型,验证结果显示,模型一致性指数(C-index)为0.909,校正曲线显示该列线图模型具有良好的区分度及一致性。
结论肺癌患者年龄、吸烟指数、TNM分期、PEF和手术时间与胸腔镜术后发生肺部感染具有密切关系,基于此建立的列线图模型对于感染高危患者的识别和降低术后并发症有一定意义。
Abstract:ObjectiveTo analyze the risk factors of lung cancer patients complicated with pulmonary infection after thoracoscopic surgery and establish a predictive nomogram model.
MethodsA total of 315 patients with primary lung cancer who had undergone thoracoscopic surgery from January 2018 to October 2021 in our hospital were divided into two groups according to the incidence of pulmonary infection. Two groups of clinical data were collected for single-factor and regression analyses, and independent predictors were obtained. On this basis, a risk model was constructed and its predictive effectiveness was evaluated.
ResultsThe independent risk factors of lung cancer patients complicated with pulmonary infection after thoracoscopic radical operation were as follows: age≥62.5 years, smoking index≥100, PEF≤72.1 ml/s, TNM stage Ⅲ/Ⅳ, and operation time≥188.5 min (P < 0.05). Based on the above factors, the risk model of the column chart was established. Model-verification results showed that the C-index of the model was 0.909, and the correction curve showed that the column chart model had good differentiation and consistency.
ConclusionLung cancer patients' age, smoking index, TNM stage, PEF, and operation time are closely related to pulmonary infection after thoracoscopic radical operation. The nomogram model is useful for identifying high-risk patients and reducing postoperative complications.
-
Key words:
- Lung infection /
- Lung cancer /
- Thoracoscopy /
- Nomogram model /
- Risk factors
-
Competing interests: The authors declare that they have no competing interests.作者贡献:张秀强:数据统计、论文撰写杨涛:论文思路整体设计
-
表 1 肺部感染组和非肺部感染组患者临床资料的单因素分析
Table 1 Univariate analysis of clinical data of patients with pulmonary infection and non-pulmonary infection

表 2 肺癌胸腔镜根治术后发生肺部感染的自变量和因变量赋值情况
Table 2 Assignment of independent variable and dependent variable in patients with lung cancer after thoracoscopic radical resection

表 3 肺癌患者胸腔镜根治术后发生肺部感染的二元Logistic回归分析
Table 3 Binary logistic regression analysis of pulmonary infection in patients with lung cancer after thoracoscopic radical resection

-
[1] Zheng R, Zhang S, Zeng H, et al. Cancer incidence and mortality in China, 2016[J]. J National Cancer Center, 2022, 2(1): 1-9. doi: 10.1016/j.jncc.2022.02.002
[2] 中华医学会, 中华医学会肿瘤学分会, 中华医学会杂志社. 中华医学会肺癌临床诊疗指南(2019版)[J]. 中华肿瘤杂志, 2020, 42(4): 257-287. doi: 10.3760/cma.j.cn112152-20200120-00049 Chinese Medical Association, Oncology Branch of Chinese Medical Association, Journal of Chinese Medical Association. Chinese Medical Association guidelines for clinical diagnosis and treatment of lung cancer (2019 edition)[J]. Zhonghua Zhong Liu Za Zhi, 2020, 42(4): 257-287. doi: 10.3760/cma.j.cn112152-20200120-00049
[3] Han D, Cao Y, Wu H, et al. Uniportal video-assisted thoracic surgery for the treatment of lung cancer: a consensus report from Chinese Society for Thoracic and Cardiovascular Surgery (CSTCVS) and Chinese Association of Thoracic Surgeons (CATS)[J]. Transl Lung Cancer Res, 2020, 9(4): 971-987. doi: 10.21037/tlcr-20-576
[4] 毛友生, 赫捷. 肺癌胸腔镜术后并发症的防治策略[J]. 中国肺癌杂志, 2018, 21(3): 230-233. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ201803024.htm Mao YS, He J. The Prevention and Management Strategy for Postoperative Complications after Thoracoscopic Surgery of Lung Cancer[J]. Zhongguo Fei Ai Za Zhi, 2018, 21(3): 230-233. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ201803024.htm
[5] 中华医学会呼吸病学分会感染学组. 中国成人医院获得性肺炎与呼吸机相关性肺炎诊断和治疗指南(2018年版)[J]. 中华结核和呼吸杂志, 2018, 41(4): 255-280. doi: 10.3760/cma.j.issn.1001-0939.2018.04.006 Chinese Medical Association Respiratory Disease Branch Infection Group. Guidelines for the diagnosis and treatment of hospital-acquired pneumonia and ventilator-associated pneumonia in adults in China (2018 edition)[J]. Zhonghua Jie He He Hu Xi Za Zhi, 2018, 41(4): 255-280. doi: 10.3760/cma.j.issn.1001-0939.2018.04.006
[6] Sabaté S, Mazo V, Canet J. Predicting postoperative pulmonary complications: implications for outcomes and costs[J]. Curr Opin Anaesthesiol, 2014, 27(2): 201-209. doi: 10.1097/ACO.0000000000000045
[7] 李鹏飞, 赖玉田, 周坤, 等. 应用Clavien-Dindo分级系统对肺癌患者术后并发症分级及危险因素分析[J]. 中国肺癌杂志, 2017, 20(4): 264-271. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ201704010.htm Li PF, Lai YT, Zhou K, et al. Analysis of Postoperative Complications and Risk Factors of Patients with Lung Cancer through Clavien-Dindo Classification[J]. Zhongguo Fei Ai Za Zhi, 2017, 20(4): 264-271. https://www.cnki.com.cn/Article/CJFDTOTAL-FAIZ201704010.htm
[8] 车强, 汪林宝, 王孝彬, 等. 胸腔镜肺癌根治术后肺部并发症发生风险分析[J]. 医学临床研究, 2020, 17(11): 1667-1670. doi: 10.3969/ji.ssn.1671-7171.2020.11.021 Che Q, Wang LB, Wang XB, et al. Risk Factors Analysis of Pulmonary Complications after Thoracoscopic Radical Resection of Lung Cancer[J]. Yi Xue Lin Chuang Yan Jiu, 2020, 17(11): 1667-1670. doi: 10.3969/ji.ssn.1671-7171.2020.11.021
[9] 徐燕, 韩啸. 肺癌胸腔镜肺切除术后并发肺部感染的危险因素分析[J]. 全科医学临床与教育, 2019, 17(11): 1010-1013. https://www.cnki.com.cn/Article/CJFDTOTAL-QKYL201911015.htm Xu Y, Han X. Risk factors of pulmonary infection after thoracoscopic surgery for lung cancer[J]. Quan Ke Yi Xue Lin Chuang Yu Jiao Yu, 2019, 17(11): 1010-1013. https://www.cnki.com.cn/Article/CJFDTOTAL-QKYL201911015.htm
[10] 张宇星, 王宇, 宋伟伟, 等. 70岁以上老年非小细胞肺癌病人术后肺部感染的危险因素研究[J]. 实用老年医学, 2019, 33(7): 661-665. doi: 10.3969/j.issn.1003-9198.2019.07.010 Zhang YX, Wang Y, Song WW, et al. Risk factors of postoperative pulmonary infections in elderly patients with non-small cell lung cancer over 70 years old[J]. Shi Yong Lao Nian Yi Xue, 2019, 33(7): 661-665. doi: 10.3969/j.issn.1003-9198.2019.07.010
[11] Dawod YT, Cook NE, Graham WB, et al. Smoking-associated interstitial lung disease: update and review[J]. Expert Rev Respir Med, 2020, 14(8): 825-834. doi: 10.1080/17476348.2020.1766971
[12] Vij N, Chandramani-Shivalingappa P, Van Westphal C, et al. Cigarette smoke-induced autophagy impairment accelerates lung aging, COPD-emphysema exacerbations and pathogenesis[J]. Am J Physiol Cell Physiol, 2018, 314(1): C73-C87. doi: 10.1152/ajpcell.00110.2016
[13] 侯海生, 王秋艳, 陈少川. 食管癌开胸术患者术后肺部感染与术前肺功能指标的相关性[J]. 国际肿瘤学杂志, 2019, V46(8): 471-474. doi: 10.3760/cma.j.issn.1673-422X.2019.08.005 Hou HS, Wang QY, Chen SC. Correlation between pulmonary infection and preoperative pulmonary function indexes in patients with esophageal cancer undergoing thoracotomy[J]. Guo Ji Zhong Liu Xue Za Zhi, 2019, V46(8): 471-474. doi: 10.3760/cma.j.issn.1673-422X.2019.08.005
[14] 蒋虹, 李隽, 童皖宁, 等. 肺功能指数对肺癌胸腔镜术后患者肺部感染的影响[J]. 中国临床医生杂志, 2018, 46(5): 576-578. doi: 10.3969/j.issn.2095-8552.2018.05.026 Jiang H, Li J, Tong WN, et al. Effect of pulmonary function index on pulmonary infection in patients with lung cancer after thoracoscopic surgery[J]. Zhongguo Lin Chuang Yi Sheng Za Zhi, 2018, 46(5): 576-578. doi: 10.3969/j.issn.2095-8552.2018.05.026
[15] 刘现海, 李峰, 孔令剑, 等. 肺功能指标对食管癌患者术后肺部感染的预测价值[J]. 中华医院感染学杂志, 2019, 29(9): 1379-1383. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY201909023.htm Liu XH, Li F, Kong LJ, et al. Value of lung function indexes in prediction of postoperative pulmonary infection in patients with esophageal cancer[J]. Zhonghua Yi Yuan Gan Ran Xue Za Zhi, 2019, 29(9): 1379-1383. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY201909023.htm
[16] 樊怿辉, 施民新, 陈赛华, 等. 呼气峰值流量对食管癌微创手术术后肺部感染的预测价值[J]. 中国临床研究, 2019, 32(8): 4. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCK201908011.htm Fan YH, Shi MX, Chen SH, et al. The predictive value of peak expiratory flow for pulmonary infection after minimally invasive surgery for esophageal cancer[J]. Zhongguo Lin Chuang Yan Jiu, 2019, 32(8): 4. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGCK201908011.htm
[17] 周建中. NSCLC患者血清PCT、D-D、SAA水平与TNM分期的关系及其对肺部感染的诊断价值[J]. 中国医学创新, 2021, 18(25): 14-17. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYCX202125006.htm Zhou JZ. Relationship between serum PCT, D-D, SAA levels and TNM staging in NSCLC patients and their diagnostic value for pulmonary infection[J]. Zhongguo Yi Xue Chuang Xin, 2021, 18(25): 14-17. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYCX202125006.htm
[18] 李乔, 范习刚. 影响肺癌化疗患者发生肺部感染的危险因素分析[J]. 实用癌症杂志, 2020, 35(1): 85-87. https://www.cnki.com.cn/Article/CJFDTOTAL-SYAZ202001024.htm Li Q, Fan XG. Analysis of risk factors affecting pulmonary infection in patients with lung cancer chemotherapy[J]. Shi Yong Ai Zheng Za Zhi, 2020, 35(1): 85-87. https://www.cnki.com.cn/Article/CJFDTOTAL-SYAZ202001024.htm
[19] 张波, 陈保富, 金将, 等. 腔镜联合食管癌根治术后合并肺部感染危险因素分析[J]. 中华医院感染学杂志, 2013, 23(6): 1349-1350, 1358. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY201306061.htm Zhang B, Chen BF, Jin J, et al. Analysis of risk factors for pulmonary infection after laparoscopy combined with radical esophagectomy[J]. Zhonghua Yi Yuan Gan Ran Xue Za Zhi, 2013, 23(6): 1349-1350, 1358. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYY201306061.htm



 下载:
下载: