-
摘要:目的
预测卵巢癌易复发因素, 分析复发性卵巢癌(ROC)患者的疗效与预后。
方法回顾性分析93例ROC患者的临床资料。采用单变量分析ROC患者无瘤生存期(DFI)影响因素。评估不同治疗方法对ROC患者无进展生存期(PFS)和复发后总生存时间(OS)的影响。
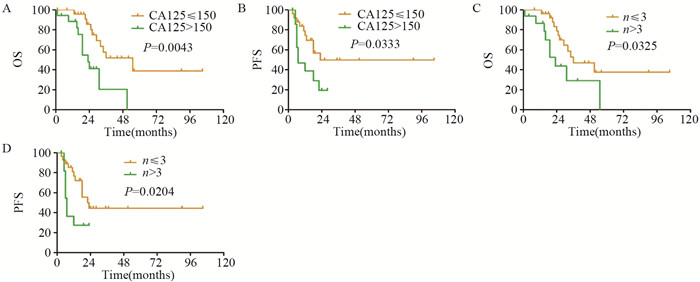
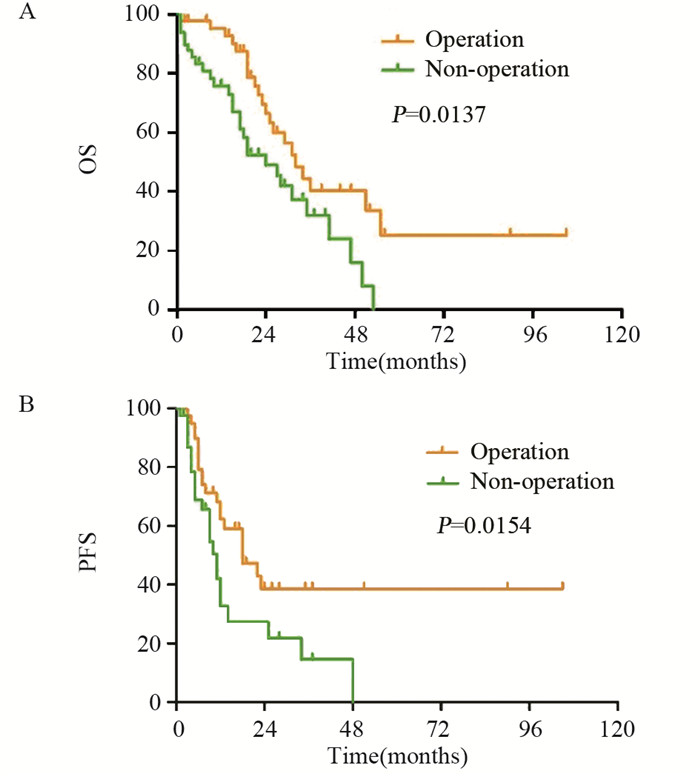
结果初次治疗后DFI单变量分析显示:肿瘤的组织分化程度、临床分期、初次术后残留肿瘤大小、初次手术后化疗疗程数与DFI有关(均P < 0.05)。93例ROC患者中, 手术组:44例患者行二次肿瘤细胞减灭术(SCS), 并联合化疗和(或)靶向治疗; 非手术组:49例患者行单纯化疗和(或)靶向治疗。手术组PFS和复发后OS均较非手术组有所延长; 手术组中:CA125 ≤ 150 U/L的患者OS和PFS较CA125>150 U/L的患者均有所延长(均P < 0.05);术前影像学检查提示复发肿瘤个数≤ 3的患者术后OS和PFS较复发肿瘤个数>3的患者均有所延长(P < 0.05)。
结论肿瘤病理分化程度越高、临床分期越早、初次术后残余病灶越小以及术后化疗疗程越规范足量的卵巢癌患者DFI越长、复发越晚。卵巢癌复发时CA125 ≤ 150 U/L、影像学检查复发肿瘤个数≤ 3的患者可能会从SCS术中获益。
Abstract:ObjectiveTo predict the recurrence of ovarian cancer (OC), to analyze the efficacy and prognosis of recurrent ovarian cancer (ROC) patients.
MethodsThe clinical medical records of 93 ROC patients were retrospectively analyzed. Univariate analysis was performed on the influencing factors of disease free interval (DFI) in ROC patients. We evaluated the effect of different treatments on progression free survival (PFS) and overall survival (OS) after recurrence.
ResultsThe single factor analysis of DFI after initial treatment showed that tumor differentiation, clinical stage, residual tumor size after initial surgery, and the number of chemotherapy courses after initial surgery were related to DFI (P < 0.05). Surgery group (n=44) were treated with secondary cytoreductive surgery (SCS) with chemotherapy and (or) targeted therapy. Non-surgery group (n=49) were treated with chemotherapy and (or) targeted therapy. PFS and OS after recurrence in surgery group were longer than those in non-surgery group. In surgery group, the patients with CA125 ≤ 150 U/L had longer OS and PFS than those with CA125>150 U/L (P < 0.05); preoperative imaging examination showed that the OS and PFS of patients with recurrent tumors number ≤ 3 were longer than those with recurrent tumors number>3 (P < 0.05).
ConclusionPathological differentiation, clinical stage, the chemotherapy course and the size of residual tumor after initial cytoreductive surgery are associated with DFI in recurrent ovarian cancer. ROC patients with recurrent tumors number ≤ 3 or CA125 ≤ 150 U/L could benefit from SCS.
-
作者贡献王娟:整理资料、分析数据、书写文章陈友国:校对数据查雪丽:收集资料周金华:指导全文
-
表 1 复发性卵巢癌患者临床病理因素影响DFI的单变量分析
Table 1 Univariate analysis of clinicopathological features on DFI of ROC patients

表 2 复发性卵巢癌患者临床病理因素影响SCS后的PFS和OS单变量分析
Table 2 Univariate analysis of clinicopathological features on PFS and OS of ROC patients after SCS

-
[1] Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012[J]. CA Cancer J Clin, 2015, 65(2):87-108. doi: 10.3322/caac.21262
[2] Takahashi A, Kato K, Matsuura M, et al. Comparison of secondary cytoreductive surgery plus chemotherapy with chemotherapy alone for recurrent epithelial ovarian, tubal, or peritoneal carcinoma:A propensity score-matched analysis of 112 consecutive patients[J]. Medicine(Baltimore), 2017, 96(37):e8006. http://cn.bing.com/academic/profile?id=5d3bca580fba92606466c230bce98f29&encoded=0&v=paper_preview&mkt=zh-cn
[3] Usami T, Kato K, Taniguchi T, et al. Recurrence patterns of advanced ovarian, fallopian tube, and peritoneal cancers after complete cytoreduction during interval debulking surgery[J]. Int J Gynecol Cancer, 2014, 24(6):991-996. doi: 10.1097/IGC.0000000000000142
[4] Ushijima K. Treatment for recurrent ovarian cancer-at first relapse[J]. J Oncol, 2010, 2010:497429. http://d.old.wanfangdata.com.cn/OAPaper/oai_pubmedcentral.nih.gov_2801501
[5] Corrado G, Salutari V, Palluzzi E, et al. Optimizing treatment in recurrent epithelial ovarian cancer[J]. Expert Rev Anticancer Ther, 2017, 17(12):1147-1158. doi: 10.1080/14737140.2017.1398088
[6] Stuart GC, Kitchener H, Bacon M, et al. 2010 Gynecologic Cancer InterGroup (GCIG) consensus statement on clinical trials in ovarian cancer:report from the Fourth Ovarian Cancer Consensus Conference[J]. Int J Gynecol Cancer, 2011, 21(4):750-755. doi: 10.1097/IGC.0b013e31821b2568
[7] van de Laar R, Zusterzeel PL, Van Gorp T, et al. Cytoreductive surgery followed by chemotherapy versus chemotherapy alone for recurrent platinum-sensitive epithelial ovarian cancer (SOCceR trial):a multicenter randomised controlled study[J]. BMC Cancer, 2014, 14:22. doi: 10.1186/1471-2407-14-22
[8] Galaal K, Naik R, Bristow RE, et al. Cytoreductive surgery plus chemotherapy versus chemotherapy alone for recurrent epithelial ovarian cancer[J]. Cochrane Database Syst Rev, 2010, (6):CD007822. http://d.old.wanfangdata.com.cn/Periodical/zlxzz201803013
[9] Harter P, Hilpert F, Mahner S, et al. Systemic therapy in recurrent ovarian cancer:current treatment options and new drugs[J]. Expert Rev Anticancer Ther, 2010, 10(1):81-88. doi: 10.1586/era.09.165
[10] Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016[J]. CA Cancer J Clin, 2016, 66(1):7-30. doi: 10.3322/caac.21332
[11] Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015[J]. CA Cancer J Clin, 2015, 65(1):5-29. doi: 10.3322/caac.21254
[12] du Bois A, Reuss A, Pujade-Lauraine E, et al. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer:a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials:by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d'Investigateurs Nationaux Pour les Etudes des Cancers de l'Ovaire (GINECO)[J]. Cancer, 2009, 115(6):1234-1244. doi: 10.1002/cncr.24149
[13] Ataseven B, Chiva LM, Harter P, et al. FIGO stage Ⅳ epithelial ovarian, fallopian tube and peritoneal cancer revisited[J]. Gynecol Oncol, 2016, 142(3):597-607. doi: 10.1016/j.ygyno.2016.06.013
[14] Kessous R, Laskov I, Abitbol J, et al. Clinical outcome of neoadjuvant chemotherapy for advanced ovarian cancer[J]. Gynecol Oncol, 2017, 144(3):474-479. doi: 10.1016/j.ygyno.2016.12.017
[15] Liu Z, Beach JA, Agadjanian H, et al. Suboptimal cytoreduction in ovarian carcinoma is associated with molecular pathways characteristic of increased stromal activation[J]. Gynecol Oncol, 2015, 139(3):394-400. doi: 10.1016/j.ygyno.2015.08.026
[16] Kyrgiou M, Salanti G, Pavlidis N, et al. Survival benefits with diverse chemotherapy regimens for ovarian cancer:meta-analysis of multiple treatments[J]. J Natl Cancer Inst, 2006, 98(22):1655-1663. doi: 10.1093/jnci/djj443
[17] Cheng X, Jiang R, Li ZT, et al. The role of secondary cytoreductive surgery for recurrent mucinous epithelial ovarian cancer (mEOC)[J]. Eur J Surg Oncol, 2009, 35(10):1105-1108. doi: 10.1016/j.ejso.2009.03.010
[18] Lorusso D, Mancini M, Di Rocco R, et al. The role of secondary surgery in recurrent ovarian cancer[J]. Int J Surg Oncol, 2012, 2012:613980. http://d.old.wanfangdata.com.cn/OAPaper/oai_pubmedcentral.nih.gov_3420128
[19] Bogani G, Rossetti D, Ditto A, et al. Artificial intelligence weights the importance of factors predicting complete cytoreduction at secondary cytoreductive surgery for recurrent ovarian cancer[J]. J Gynecol Oncol, 2018, 29(5):e66. doi: 10.3802/jgo.2018.29.e66
[20] Giudice MT, D'Indinosante M, Cappuccio S, et al. Secondary cytoreduction in ovarian cancer:who really benefits?[J]. Arch Gynecol Obstet, 2018, 298(5):873-879. doi: 10.1007/s00404-018-4915-1
[21] Oza AM, Cook AD, Pfisterer J, et al. Standard chemotherapy with or without bevacizumab for women with newly diagnosed ovarian cancer (ICON7):overall survival results of a phase 3 randomised trial[J]. Lancet Oncol, 2015, 16(8):928-936. doi: 10.1016/S1470-2045(15)00086-8
[22] Guo N, Peng Z. Does serum CA125 have clinical value for follow-up monitoring of postoperative patients with epithelial ovarian cancer? Results of a 12-year study[J]. J Ovarian Res, 2017, 10(1):14. doi: 10.1186/s13048-017-0310-y
[23] Rustin GJ, van der Burg ME, Griffin CL, et al. Early versus delayed treatment of relapsed ovarian cancer (MRC OV05/EORTC 55955):a randomised trial[J]. Lancet, 2010, 376(9747):1155-1163. doi: 10.1016/S0140-6736(10)61268-8
[24] Parashkevova A, Sehouli J, Richter R, et al. Preoperative CA-125 Value as a Predictive Factor for Postoperative Outcome in First Relapse of Platinum-sensitive Serous Ovarian Cancer[J]. Anticancer Res, 2018, 38(8):4865-4870. doi: 10.21873/anticanres.12799
[25] Onda T, Yoshikawa H, Yasugi T, et al. Secondary cytoreductive surgery for recurrent epithelial ovarian carcinoma:proposal for patients selection[J]. Br J Cancer, 2005, 92(6):1026-1032. doi: 10.1038/sj.bjc.6602466
[26] Bristow RE, Peiretti M, Gerardi M, et al. Secondary cytoreductive surgery including rectosigmoid colectomy for recurrent ovarian cancer:operative technique and clinical outcome[J]. Gynecol Oncol, 2009, 114(2):173-177. doi: 10.1016/j.ygyno.2009.05.004
[27] Zang RY, Harter P, Chi DS, et al. Predictors of survival in patients with recurrent ovarian cancer undergoing secondary cytoreductive surgery based on the pooled analysis of an international collaborative cohort[J]. Br J Cancer, 2011, 105(7):890-896. doi: 10.1038/bjc.2011.328
[28] Harter P, Beutel B, Alesina PF, et al. Prognostic and predictive value of the Arbeitsgemeinschaft Gynaekologische Onkologie (AGO) score in surgery for recurrent ovarian cancer[J]. Gynecol Oncol, 2014, 132(3):537-541. doi: 10.1016/j.ygyno.2014.01.027
[29] Loizzi V, Del Vecchio V, Gargano G, et al. Biological Pathways Involved in Tumor Angiogenesis and Bevacizumab Based Anti-Angiogenic Therapy with Special References to Ovarian Cancer[J]. Int J Mol Sci, 2017, 18(9). pii:E1967. doi: 10.3390/ijms18091967
[30] Basu P, Mukhopadhyay A, Konishi I. Targeted therapy for gynecologic cancers:Toward the era of precision medicine[J]. Int J Gynaecol Obstet, 2018, 143 Suppl 2:131-136. http://cn.bing.com/academic/profile?id=fe1cb866d8c6d754ffafc0f7b9c4ef03&encoded=0&v=paper_preview&mkt=zh-cn
[31] Heo YA, Duggan ST. Niraparib:A Review in Ovarian Cancer[J]. Target Oncol, 2018, 13(4):533-539. doi: 10.1007/s11523-018-0582-1



 下载:
下载: