Relationship of Para-aortic Lymph Nodes (PALN) Status with Prognosis and Clinicopathological Features of Pancreatic Cancer Patients After Pancreatectomy
-
摘要:目的
探讨胰腺癌患者胰腺切除术后16组淋巴结状态与其预后及临床病理特征的关系。
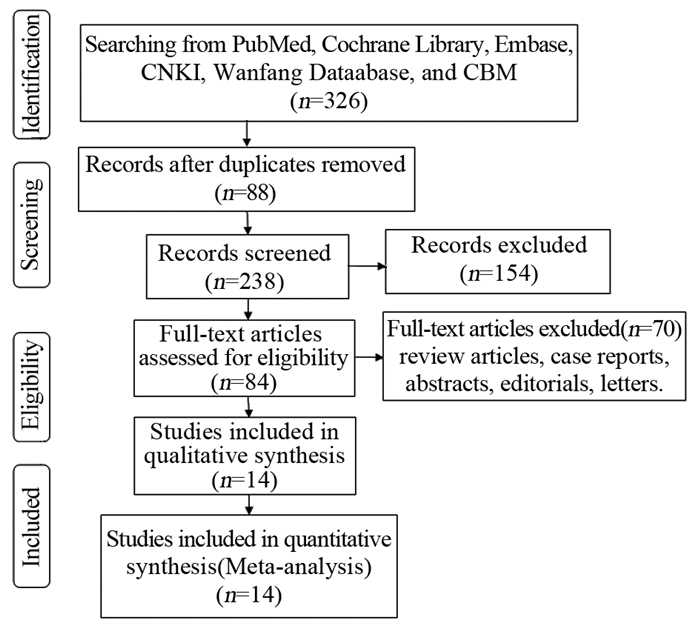
方法检索PubMed数据库、Cochrane Library、Embase数据库、CNKI数据库、万方数据库及中国生物医学文献(CBM)数据库,均从建库开始截至2016年7月,查找胰腺癌患者行胰腺切除术后腹主动脉旁淋巴结(para-aortic lymph noldes,PALN)病理检查结果与患者临床病理特征及生存率相关文献,采用Stata 12.0软件进行Meta分析。
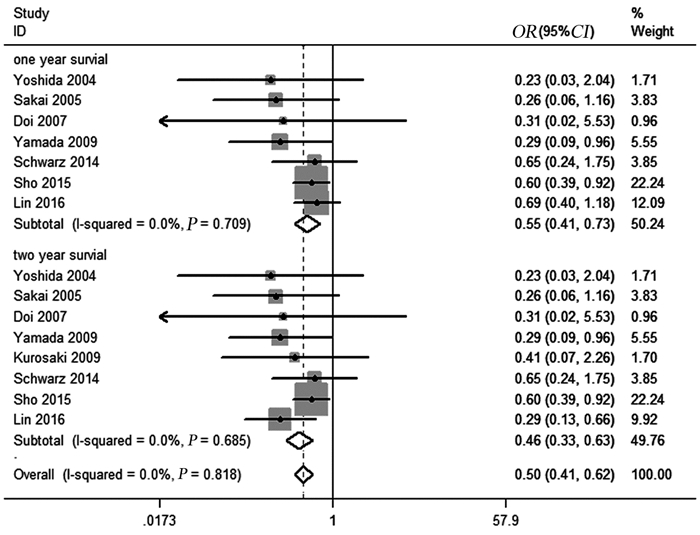
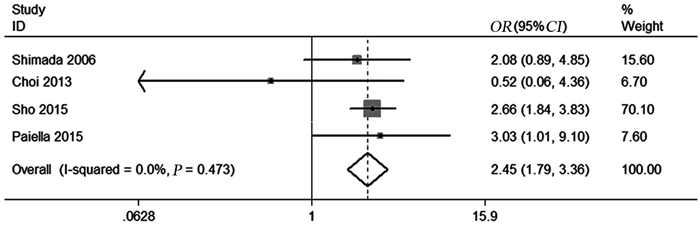
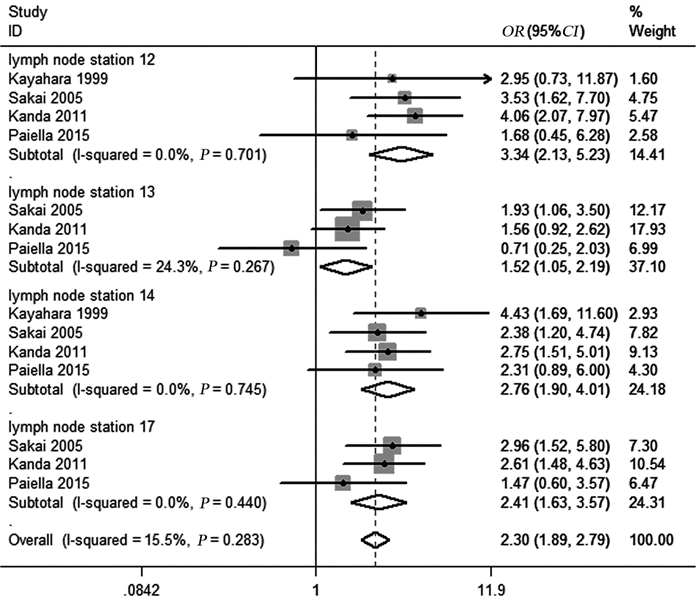
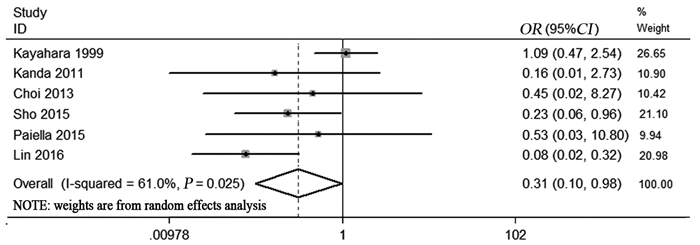
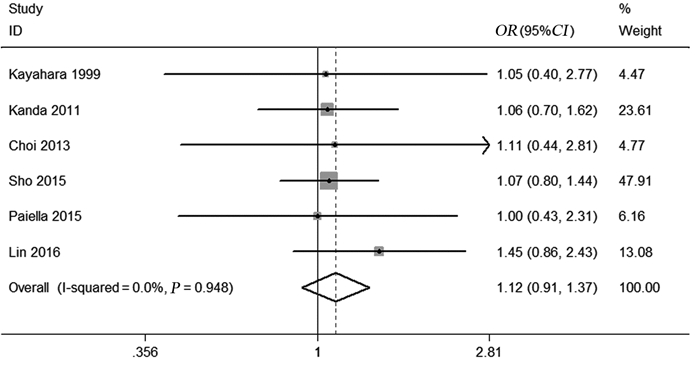
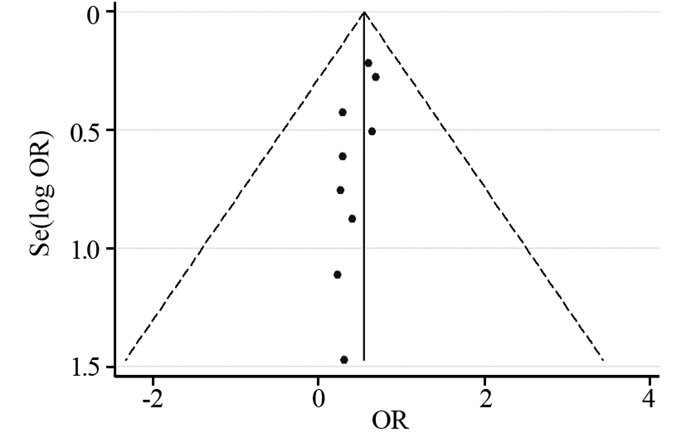
结果共纳入14项研究,其中回顾性研究12项,前瞻性研究2项,涉及胰腺癌患者3 279人。Meta分析结果显示,PALN阳性患者1年生存率(OR=0.55,95%CI:0.41~0.73,P=0.001)和2年生存率(OR=0.46,95%CI:0.33~0.63,P=0.001)均明显低于PALN阴性患者,同时提示PALN阳性可能会增加切缘阳性的风险(OR=2.45,95%CI:1.79~3.36,P=0.001)。在其他组淋巴结转移方面,PALN病理检查阳性会增加12组(OR=3.34,95%CI:2.13~5.23,P=0.001)、14组(OR=2.76,95%CI:1.90~4.01,P=0.001)、17组(OR=2.41,95%CI:1.63~3.57,P=0.001)淋巴结转移的风险。在T分期方面,胰腺癌PALN阳性患者T1/T2期所占比例低于PALN阴性患者(OR=0.31,95%CI:0.10~0.98,P=0.046)。
结论胰腺癌患者行胰腺切除术后,腹主动脉旁淋巴结阳性患者近期生存率低,手术切缘阳性的风险较高,远处转移的可能较大。PALN状态与胰腺癌患者预后及临床病理特征相关。
Abstract:ObjectiveTo explore the relationship of para-aortic lymph nodes (PALN) status with prognosis and clinicopathological features of pancreatic carcinoma patients after pancreatectomy.
MethodsPubMed, Cochrane Library, Embase, CNKI, Wanfang Database and CBM were searched to identify the studies reporting the relationship of PALN with clinicopathological features and short-term survival of pancreatic cancer patients after pancreatectomy from inception to July 2016. Meta-analysis was performed by Stata 12.0 software.
ResultsA total of 14 studies were included, involving 3279 pancreatic cancer patients. Patients with positive PALN had worse one-year (OR=0.55, 95%CI:0.41-0.73, P=0.001) and two-year (OR=0.46, 95%CI:0.33-0.63, P=0.001) survival than those with negative PALN. Positive PALN was associated with increased possibility of R1 resection(OR=2.45, 95%CI:1.79-3.36, P=0.001), station 12 (OR=3.34, 95%CI:2.13-5.23, P=0.001), station 14(OR=2.76, 95%CI:1.90-4.01, P=0.001) and station 17 (OR=2.41, 95%CI:1.63-3.57, P=0.001) malignant infiltration, and decreased T1/T2 stage percentage(OR=0.31, 95%CI:0.10-0.98, P=0.046).
ConclusionThe pancreatic cancer patients with positive PALN may suffer from a low short-term survival, high possibility of positive margin resection and malignant infiltration. PALN status is associated with clinicopathological features and prognosis of pancreatic cancer patients.
-
Key words:
- Pancreatic Cancer /
- Pancreatectomy /
- Para-aortic lymph nodes /
- Station 16 lymph nodes /
- Meta-analysis
-
-
表 1 纳入文献中胰腺癌患者的基本特征
Table 1 Characteristics of pancreatic cancer patients in the included studies

-
[1] Garrido-Laguna I, Hidalgo M. Pancreatic cancer:from state-of-the-art treatments to promising novel therapies[J]. Nat Rev Clinl Oncol, 2015, 12(6):319-34. doi: 10.1038/nrclinonc.2015.53
[2] DeSantis CE, Siegel RL, Sauer AG, et al. Cancer statistics for African Americans, 2016:Progress and opportunities in reducing racial disparities[J]. CA Cancer J Clin, 2016, 66(4):290-308. doi: 10.3322/caac.v66.4
[3] Chen W. Cancer statistics:updated cancer burden in China[J]. Chin J Cancer Res, 2015, 27(1):1. https://www.ncbi.nlm.nih.gov/pubmed/?term=Cancer+statistics%3A+updated+cancer+burden+in+China
[4] Ma Q. Perineural invasion and pancreatic cancer[J]. Pancreatology, 2016, 16(1):S28.
[5] Hidalgo M. Pancreatic cancer[J]. N Engl Jf Med, 2010, 362(17):1605-17. doi: 10.1056/NEJMra0901557
[6] 杨尹默.胰腺癌外科治疗的现状、存在问题与展望[J].中国普通外科杂志, 2016, 25(9):1231-5. doi: 10.3978/j.issn.1005-6947.2016.09.001 Yang YM. Surgical managements of pancreatic cancer:current status and future directions[J]. Zhongguo Pu Tong Wai Ke Za Zhi, 2016, 25(9):1231-5. doi: 10.3978/j.issn.1005-6947.2016.09.001
[7] 陈博滔, 陈梅福.交界性可切除胰腺癌的研究进展[J].中国普通外科杂志, 2016, 25(3):448-55. doi: 10.3978/j.issn.1005-6947.2016.03.025 Chen BT, Chen MF. Research progress of borderline resectable pancreatic cancer[J]. Zhongguo Pu Tong Wai Ke Za Zhi, 2016, 25(3):448-55. doi: 10.3978/j.issn.1005-6947.2016.03.025
[8] Tol JA, Gouma DJ, Bassi C, et al. Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma:A consensus statement by the International Study Group on Pancreatic Surgery (ISGPS)[J]. Surgery, 2014, 156(3):591-600. doi: 10.1016/j.surg.2014.06.016
[9] Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses[J]. Eur J Epidemiol, 2010, 25(9):603-5. doi: 10.1007/s10654-010-9491-z
[10] Kayahara M, Nagakawa T, Ohta T, et al. Analysis of paraaortic lymph node involvement in pancreatic carcinoma[J]. Cancer, 1999, 85(3):583-90. doi: 10.1002/(ISSN)1097-0142
[11] Yoshida T, Matsumoto T, Sasaki A, et al. Outcome of paraaortic node-positive pancreatic head and bile duct adenocarcinoma[J]. Am J Surg, 2004, 187(6):736-40. doi: 10.1016/j.amjsurg.2003.07.031
[12] Sakai M, Nakao A, Kaneko T, et al. Para-aortic lymph node metastasis in carcinoma of the head of the pancreas[J]. Surgery, 2005, 137(1):606-11.
[13] Shimada K, Sakamoto Y, Sano T, et al. The role of paraaortic lymph node involvement on early recurrence and survival after macroscopic curative resection with extended lymphadenectomy for pancreatic carcinoma[J]. J Am Coll Surg, 2006, 203(3):345-52. doi: 10.1016/j.jamcollsurg.2006.05.289
[14] DoiR, Kami K, Ito D, et al. Prognostic implication of para-aortic lymph node metastasis in resectable pancreatic cancer[J]. World J Surg, 2007, 31(1):147-54. doi: 10.1007/s00268-005-0730-5
[15] Yamada S, Nakao A, Fujii T, et al. Pancreatic cancer with paraaortic lymph node metastasis:a contraindication for radical surgery?[J]. Pancreas, 2009, 38(1):e13-7. doi: 10.1097/MPA.0b013e3181889e2d
[16] Kurosaki I, Kawachi Y, Nihei K, et al. Liver perfusion chemotherapy with 5-Fluorouracil followed by systemic gemcitabine administration for resected pancreatic cancer:preliminary results of a prospective phase 2 study[J]. Pancreas, 2009, 38(2):161-7. doi: 10.1097/MPA.0b013e31818815f7
[17] Kanda M, Fujii T, Nagai S, et al. Pattern of lymph node metastasis spread in pancreatic cancer[J]. Pancreas, 2011, 40(6):951-5. doi: 10.1097/MPA.0b013e3182148342
[18] Choi SH, Kim SH, Choi JJ, et al. Clinical necessity of the immunohistochemical reassessment of para-aortic lymph nodes in resected pancreatic ductal adenocarcinoma[J]. Oncol Lett, 2013, 6(5):1189-94. https://www.jove.com/visualize?author=K+Kim
[19] Schwarz L, Lupinacci RM, Svrcek M, et al. Para-aortic lymph node sampling in pancreatic head adenocarcinoma[J]. Br J Surg, 2014, 101(5):530-8. doi: 10.1002/bjs.2014.101.issue-5
[20] Sho M, Murakami Y, Motoi F, et al. Postoperative prognosis of pancreatic cancer with para-aortic lymph node metastasis:a multicenter study on 822 patients[J]. J Gastroenterol, 2015, 50(6):694-702. doi: 10.1007/s00535-014-1005-4
[21] Paiella S, Malleo G, Maggino L, et al. Pancreatectomy with Para-Aortic Lymph Node Dissection for Pancreatic Head Adenocarcinoma:Pattern of Nodal Metastasis Spread and Analysis of Prognostic Factors[J]. J Gastrointest Surg, 2015, 19(9):1610-20. doi: 10.1007/s11605-015-2882-4
[22] Liu C, Yu L, Luo G, et al. Which patients with para-aortic lymph node (LN16) metastasis will truly benefit from curative pancreaticoduodenectomy for pancreatic head cancer?[J]. Oncotarget, 2016, 7(20):29177-86. doi: 10.18632/oncotarget.v7i20
[23] Lin JY, Zhang XM, Kou JT, et al. Analysis of prognostic factors for pancreatic head cancer according to para-aortic lymph node[J]. Cancer Med, 2016, 5(10):2701-7. doi: 10.1002/cam4.2016.5.issue-10
[24] 黄江, 白利杰, 张生军, 等.局部切除胰体尾联合血管切除重建治疗晚期胰腺癌的疗效分析[J].中国普通外科杂志, 2016, 25(9):1253-8. doi: 10.3978/j.issn.1005-6947.2016.09.005 Huang J, Bai LK, Zhang SJ, et al. Efficacy analysis of local resection of the body and tail of the pancreas combined with vascular resection and reconstruction for advanced pancreatic cancer[J]. Zhongguo Pu Tong Wai Ke Za Zhi, 2016, 25(9):1253-8. doi: 10.3978/j.issn.1005-6947.2016.09.005
[25] Clancy TE. Surgery for pancreatic cancer[J]. Hematol Oncol Clin North Am, 2015, 29(4):701-16. doi: 10.1016/j.hoc.2015.04.001
[26] Gall TM, Tsakok M, Wasan H, et al. Pancreatic cancer:current management and treatment strategies[J]. Postgrad Med J, 2015, 91(1080):601-7. doi: 10.1136/postgradmedj-2014-133222
[27] Agalianos C, Gouvas N, Papaparaskeva K, et al. Positive para-aortic lymph nodes following pancreatectomy for pancreatic cancer. Systematic review and meta-analysis of impact on short term survival and association with clinicopathologic features[J]. HPB (Oxford), 2016, 18(8):633-41. doi: 10.1016/j.hpb.2016.04.007
[28] Paiella S, Sandini M, Gianotti L, et al. The prognostic impact of para-aortic lymph node metastasis in pancreatic cancer:A systematic review and meta-analysis[J]. Eur J Surg Oncol, 2016, 42(5):616-24. doi: 10.1016/j.ejso.2016.02.003
[29] Sohal DP, Mangu PB, Laheru D. Metastatic pancreatic cancer:American society of clinical oncology clinical practice guideline summary[J]. J Oncol Pract, 2017, 13(4):261-4. doi: 10.1200/JOP.2016.017368
[30] Maemura K, Takao S, Shinchi H, et al. Role of positron emission tomography in decisions on treatment strategies for pancreatic cancer[J]. J Hepatobiliary Pancreatic Sury, 2006, 13(5):435-41. doi: 10.1007/s00534-006-1102-8
[31] Gaedcke J, Gunawan B, Grade M, et al. The mesopancreas is the primary site for R1 resection in pancreatic head cancer:relevance for clinical trials[J]. Langenbeck Arch Surg, 2010, 395(4):451-8. doi: 10.1007/s00423-009-0494-8
[32] Rahbari NN, Bork U, Motschall E, et al. Molecular detection of tumor cells in regional lymph nodes is associated with disease recurrence and poor survival in node-negative colorectal cancer:a systematic review and meta-analysis[J]. J Clinl Oncol, 2012, 30(1):60-70. doi: 10.1200/JCO.2011.36.9504
[33] Strobel O, Hank T, Hinz U, et al. Pancreatic cancer surgery:the new r-status counts[J]. Ann Surg, 2017, 265(3):565-73. doi: 10.1097/SLA.0000000000001731



 下载:
下载: