133 Effect of Different Biliary Drainage Methods in Treatment of Malignant High Biliary Obstruction
-
摘要:目的
探讨不同胆道引流方式对高位恶性胆道梗阻(malignant high biliary obstruction, MHBO)疗效的影响,为临床治疗方式的选择提供参考。
方法随访MHBO患者164例,其中行胆道完全外引流18例(A组)、胆道单支架植入并对侧外引流48例(B组)、胆道优势侧引流34例(C组)、胆道双支架植入64例(D组),观察术后近、远期疗效。
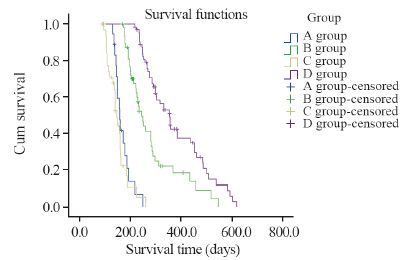
结果4组患者术前ALT、AST、TBIL、DBIL与术后第3、7、14天比较,差异均有统计学意义(均P<0.05);4组患者术后第7天的组间比较,A、B、D三组下降程度高于C组,差异均有统计学意义(均P<0.05);4组患者术后第14天的组间比较,D组下降程度明显高于A、B、C三组,B组高于A、C两组,A组高于C组,差异均有统计学意义(均P<0.05)。4组患者术后第21天TBIL均值与术前比较,D组下降程度明显高于A、B、C三组,B组高于A、C两组,A组高于C组,差异均有统计学意义(均P<0.05)。4组患者术后生存期比较,D组中位生存期为(355.00±22.21)天,远高于A、B、C三组,差异均有统计学意义(均P<0.05)。
结论胆道双支架植入实现了胆汁的充分内引流,对迅速消除黄疸具有明显的优越性,明显的提高了患者的生存质量及延长了生存期。
Abstract:ObjectiveTo explore the correlation of different biliary drainage methods with curative effect in the treatment of malignant high biliary obstruction(MHBO).
MethodsA retrospective investigation was performed in 164 patients diagnosed as MHBO in the Fourth Hospital of Hebei Medical University. Among them, 18 cases received complete external drainage of biliary tract(group A), 48 cases received biliary single stent implantation combined with lateral drainage(group B), 34 cases received external drainage of biliary tract(group C), and 64 cases received biliary double stent implantation(group D). The short-term and long-term therapeutic evaluations as well as the postoperative complications were observed.
ResultsThe differences in ALT, AST, TBIL and DBIL of all patients before operation and the 3rd, 7th, 14th day after operation were significant (P<0.05); on the 7th day, the decreased degree in the levels of ALT, AST, TBIL and DBIL in group A, B, D were higher than those in group C (P<0.05); on the 14th day, the decreased degree in the levels of ALT, AST, TBIL and DBIL in group D were higher than those in the other three groups, while they were higher in group B compared with group A and C, higher in group A than in group C (all P<0.05); on the 21st day, the decreased degree in the level of TBIL in group D was higher than those in the other three groups, while it was higher in group B compared with group A and C, higher in group A than in group C (all P<0.05). The postoperative median survival time of group D[(355.00±22.21)days] was obviously longer than the other three groups (P<0.05). C onclusion Reasonable drainage method can significantly improve the symptoms of the patients with malignant high biliary obstruction. Biliary double stent implantation can achieve adequate internal drainage, which has obvious advantages in rapid elimination of jaundice, and it is worthy of clinical promotion.
-
Key words:
- Biliary tract obstructive /
- Biliary drainage /
- Stent implantation /
- Curative effect
-
-
表 1 4组高位恶性胆道梗阻患者术前、术后肝功能变化情况 (x±s)
Table 1 Changes of liver function before and after operation in 4 groups of malignant high biliary obstruction patients (x±s)

表 2 4组高位恶性胆道梗阻患者术前及术后第21天TBIL变化情况 (x±s)
Table 2 Changes of TBIL before operation and 21 days after operation in 4 groups of malignant high biliary obstruction patients (x±s)

表 3 4组高位恶性胆道梗阻患者术中及术后并发症
Table 3 Intraoperative and postoperative complications of 4 groups of malignant high biliary obstruction patients

-
[1] Wang Y, Yang H, Shen C, et a1. Surgical procedure and long-term survival of hilar cholangiocarcinoma[J]. Int J Clin Exp Med, 2015, 8(1): 1122-8.
[2] 武中林, 单保恩, 李顺宗, 等. 高位恶性胆道梗阻胆道双支架植入的疗效[J]. 肿瘤防治研究, 2015, 42(5): 498-501. http://www.zlfzyj.com/CN/article/searchArticleResult.do# Wu ZL, Shan BE, LI SZ, et al. Efficacy of biliary double stents implant on malignant high biliary obstruction[J]. Zhong Liu Fang Zhi Yan Jiu, 2015, 42(5): 498-501. http://www.zlfzyj.com/CN/article/searchArticleResult.do#
[3] 李明武, 殷占新, 韩国宏. 经皮肝穿胆道引流术治疗恶性梗阻性黄疽的临床应用现状[J]. 介入放射学杂志, 2013, 22(10): 877-80. http://www.cnki.com.cn/Article/CJFDTOTAL-JRFS201310026.htm Li MW, Yin ZX, Han GH. The current clinical practice of percutaneous transhepatic biliary drainage for the treatment of malignant biliary obstruction[J]. Jie Ru Fang She Xue Za Zhi, 2013, 22(10): 877-80. http://www.cnki.com.cn/Article/CJFDTOTAL-JRFS201310026.htm
[4] Choi J, Ryu JK, Lee SH, et al. Biliary drainage for obstructive jaundice caused by unresectable hepatocellular carcinoma:the endoscopic versus percutaneous approach[J]. Hepatobiliary Pancreat Dis Int, 2012, 11(6): 636-42. doi: 10.1016/S1499-3872(12)60237-9
[5] Shweel MAG, Othman MHM, Mourad AF, et al. New modification of deep biliary cannulation using endoscopic-radiologic rendezvous technique for palliative treatment of malignant obstructive jaundice[J]. Egyptian Radiol Nucl Med, 2012, 43(4): 555-9. doi: 10.1016/j.ejrnm.2012.09.003
[6] 李鹏, 向贤宏, 蔡春芳, 等. 经皮经肝胆管引流术不同术式治疗恶性梗阻性黄疸临床疗效分析[J]. 实用医学杂志, 2013, 29(11): 1762-4. http://www.cnki.com.cn/Article/CJFDTOTAL-SYYZ201311018.htm Li P, Xiang XH, Cai CF, et al. Clinical efficacy of the treatment of malignant obstructive jaundice with percutaneous transhepatic cholangiography and biliary drainage (PTCD)[J]. Shi Yong Yi Xue Za Zhi, 2013, 29(11): 1762-4. http://www.cnki.com.cn/Article/CJFDTOTAL-SYYZ201311018.htm
[7] Iwano H, Ryozawa S, Ishigaki N, et al. Unilateral versus bilateral drainage using self-expandable metallic stmt for unresectable hilar biliary obstruction[J]. Dig Endosc, 2011, 23(1): 43-8. doi: 10.1111/den.2011.23.issue-1
[8] 杨丽, 王俊梅, 姜海波, 等. 恶性梗阻性黄疸的两种微创介入治疗术后并发症比较分析[J]. 中国现代医生, 2015, 53(2): 36-8. http://www.cnki.com.cn/Article/CJFDTOTAL-ZDYS201502014.htm Yang L, Wang JM, Jiang HB, et al. Comparison of postoperative complication rate between two kinds of minimally invasive treatment for malignant obstructive jaundice[J]. Zhongguo Xian Dai Yi Sheng, 2015, 53(2): 36-8. http://www.cnki.com.cn/Article/CJFDTOTAL-ZDYS201502014.htm
[9] 武中林, 刘玉芝, 刘亮, 等. 超声引导联合右侧单通道胆道双支架植入治疗高位恶性胆道梗阻[J]. 中华超声影像学杂志, 2015, 24(3): 264-5. Wu ZL, Liu YZ, Liu L, et al. Single-channel dual stents in the treatment of malignant high biliary obstruction[J]. Zhonghua Chao Sheng Ying Xiang Xue Za Zhi, 2015, 24(3): 264-5.
[10] Lawson AJ, Beningfield SJ, Kfige JE, et al. Percutaneous transhepatic self-expanding metal stents for palliation of malignant biliary obstruction[J]. S Afr J Surg, 2012, 50(3): 54-8.
[11] Gümüş M1, Celebi F, Böyük A, et al. Dehydroepiandrosterone ameliorates hepatocellular damage in obstructive jaundice[J]. Cell Biochem Funct, 2010, 28(6): 515-20. doi: 10.1002/cbf.1686
[12] 杨琦, 陈之强, 彭正. 经皮肝穿胆道支架植入术治疗恶性梗阻性黄疸的研究[J]. 中华全科医学, 2013, 11(1): 82-3. http://www.cnki.com.cn/Article/CJFDTOTAL-SYQY201301045.htm Yang Q, Chen ZQ, Peng Z. The study of percutaneous transhepatic insertion of biliary stent in treating malignant biliary obstruction[J]. Zhong hua Quan Ke Yi Xue, 2013, 11(1): 82-3. http://www.cnki.com.cn/Article/CJFDTOTAL-SYQY201301045.htm
[13] 李洪义, 何东风, 张启暝. 单通道双支架置入治疗梗阻性黄疸的临床研究[J]. 现代肿瘤医学, 2015, 23(8): 1094-6. http://www.cnki.com.cn/Article/CJFDTOTAL-SXZL201508020.htm Li HY, He DF, Zhang QM. Analysisof double stents placed in treatment of patients withobstructive jaundice by one-sided biliary puncture[J].Xian Dai Zhong Liu Yi Xue, 2015, 23(8): 1094-6. http://www.cnki.com.cn/Article/CJFDTOTAL-SXZL201508020.htm
[14] 杨福玲, 苏洪英, 冯博, 等. 肝门部胆管癌单双侧引流介入治疗疗效对比分析[J]. 介入放射学杂志, 2009, 18(8): 603-6. http://www.cnki.com.cn/Article/CJFDTOTAL-JRFS200908015.htm Yang FL, Su HY, Feng B, et al. The efficacy of interventional therapy for hilar cholangiocaarcinoma: a comparison between unilateral and bilateral duct drainage[J]. Jie Ru Fang She Xue Za Zhi, 2009, 18(8): 603-6. http://www.cnki.com.cn/Article/CJFDTOTAL-JRFS200908015.htm
[15] 王庆华, 管清海, 陈强谱. 早期生态免疫肠内营养对梗阻性黄疸患者术后免疫和肠黏膜屏障的影响[J]. 中国老年学杂志, 2015, 35(6): 1522-4. http://www.cnki.com.cn/Article/CJFDTOTAL-ZLXZ201506043.htm Wang QH, Guang QH, Chen QP. Effect of early enteral nutrition on immune function and intestinal mucosal barrier in patients with obstructive jaundice[J]. Zhongguo Lao Nian Xue Za Zhi, 2015, 35(6): 1522-4. http://www.cnki.com.cn/Article/CJFDTOTAL-ZLXZ201506043.htm
[16] 王文君, 于聪慧. 胆道支架引流术对恶性梗阻性黄疸患者肝功能的影响[J]. 临床肝胆病杂志, 2015, 31(8): 1295-8. http://www.cnki.com.cn/Article/CJFDTOTAL-LCGD201508037.htm Wang WJ, Yu CH. Improvement in liver function in patients with malignant obstructive jaundice after endoscopic biliary metallic stent drainage[J]. Lin Chuang Gan Dan Bing Za Zhi, 2015, 31(8): 1295-8. http://www.cnki.com.cn/Article/CJFDTOTAL-LCGD201508037.htm
[17] 朱林忠, 赵永军, 朱旭, 等. 介人治疗恶性胆道梗阻时胆心反射的防治[J]. 中华肝胆外科杂志, 2013, 19(5): 388-9. Zhu LZ, Zhao YJ, Zhu X, et al. Prevention and treatment of biliary cardiac reflex in interventional treatment of malignant biliary obstruction[J].Zhonghua Gan Dan Wai Ke Za Zhi, 2013, 19(5): 388-9.
[18] Kawashima H, Itoh A, Ohno E, et al. Preoperative endoscopicnasobiliary drainage in 164 consecutive patients with suspected perihilar cholangiocarcinoma: a retrospective study of efficacy and risk factors related tocomplications[J]. Ann Surg, 2013, 257(1): 121-7. doi: 10.1097/SLA.0b013e318262b2e9
[19] 赵亮, 陈强谱. 梗阻性黄疸与肠道菌群失调[J].中华临床医师杂志(电子版), 2015, 9(15): 2920-5. http://www.cnki.com.cn/Article/CJFDTOTAL-ZLYD201515031.htm Zhao L, Chen QP. Study of obstructive jaundice and intestinal floraimbalance[J]. Zhonghua Lin Chuang Yi Shi Za Zhi(Dian Zi Ban), 2015, 9(15): 2920-5. http://www.cnki.com.cn/Article/CJFDTOTAL-ZLYD201515031.htm
[20] 贾一平, 茅爱武, 蒋霆辉, 等. 梗阻性黄疸经皮肝穿刺胆道引流感染发生因素的探讨[J]. 东南大学学报(医学版), 2015, 34(3): 352-6. http://www.cnki.com.cn/Article/CJFDTOTAL-NJTD201503004.htm Jia YP, Mao AW, Jiang TH, et al. Discussion on infection factors of percutaneous liver biopsybiliary drainage in treatment to obstructive jaundice[J]. Dongnan Da Xue Xue Bao(Yi Xue Bao), 2015, 34(3): 352-6. http://www.cnki.com.cn/Article/CJFDTOTAL-NJTD201503004.htm
[21] 张汉洋, 庄志彬. 经皮肝穿刺胆管引流术联合金属支架置入姑息性治疗恶性胆道梗阻的效果分析[J].中国普通外科杂志, 2015, 24(8): 1145-9. http://www.cnki.com.cn/Article/CJFDTOTAL-ZPWZ201508025.htm Zhang HY, Zhuang ZB.Efficacy analysis of percutaneous transhepatic cholangial drainage plus metal stent placement in palliative treatment of malignant biliary obstruction[J]. Zhongguo Pu Tong Wai Ke Za Zhi, 2015, 24(8): 1145-9. http://www.cnki.com.cn/Article/CJFDTOTAL-ZPWZ201508025.htm



 下载:
下载:

