文章信息
- 郑慧琳,陈宇静,郑潇,邵丹,李晶,陈立.
- ZHENG Huilin, CHEN Yujing, ZHENG Xiao, SHAO Dan, LI Jing, CHEN Li.
- “凤凰涅槃”通路与肿瘤的复发和转移
- Phoenix Rising’ Pathway on Tumor Recurrence and Metastasis
- 肿瘤防治研究, 2015, 42(11): 1161-1164
- Cancer Research on Prevention and Treatment, 2015, 42(11): 1161-1164
- http://www.zlfzyj.com/CN/10.3971/j.issn.1000-8578.2015.11.023
-
文章历史
- 收稿日期: 2014-10-21
- 修回日期: 2015-02-11
抑制恶性肿瘤的复发和转移一直是肿瘤治疗的棘手问题。肿瘤患者经手术、化疗和放疗等综合治疗后,病情得以缓解,但仍会复发,且复发瘤较原发瘤生长快,对再次化疗和放疗敏感度降低甚至抵抗,进而更容易转移,成为肿瘤患者死亡的主要原因。这一普遍现象引导我们必须思考这样的问题:放疗和化疗本身是否可能成为复发和转移的启动因素呢?被杀死或凋亡的肿瘤细胞在复发和转移中扮演什么样的角色呢?虽然大量研究表明肿瘤复发和转移是涉及一系列基因调控的多步骤的复杂过程, 包括细胞的再增殖、黏附、基质降解、细胞迁移以及肿瘤血管生成等多个环节,但经治疗后残存的肿瘤细胞是如何获得再次大量增殖能力,即肿瘤细胞 “凤凰涅槃” 的机制并不清楚。因此,本文结合文献试图寻找肿瘤细胞“凤凰涅槃”的启动因素及肿瘤复发和转移的关系,为临床肿瘤防治提供新策略和新思路。
1 “凤凰涅槃”现象与肿瘤微环境肿瘤微环境是肿瘤细胞产生和生活的内环境,由多种细胞、胞外基质和胞外分子组成,研究表明大部分肿瘤复发时微环境都发生改变,会导致大量的癌基因活化及抑癌基因的失活,从而促进肿瘤细胞的再增殖[1, 2]。因此,肿瘤微环境作为保护和支持肿瘤复发的理论已为多数学者所接受。近年来证实,肿瘤放、化疗后引起肿瘤微环境的炎症介质,如生长因子、细胞趋化因子和免疫因子产生,利于肿瘤的增殖、侵袭、黏附、血管生成以及对放化疗的抵抗,促使恶性肿瘤的复发和转移[3]。因此将肿瘤放疗或者化疗中,濒死的肿瘤细胞通过旁分泌释放大量的炎症介质至肿瘤微环境,从而促进临近残余的、未被杀死的肿瘤细胞再增殖的现象称为“凤凰涅槃”,但引起“凤凰涅槃”的启动因素和信号通路尚不清晰[4, 5, 6]。
2 凋亡执行蛋白活化“凤凰涅槃”通路Huang等[7]研究结果证实半胱氨酸蛋白酶-3(cysteine aspartic acid specific protease-3,Caspase-3)作为细胞凋亡级联反应的执行者在肿瘤的复发中扮演了重要的角色。研究者们发现放疗、化疗导致肿瘤细胞凋亡的过程中,濒死的肿瘤细胞具有强烈刺激残存的肿瘤细胞增殖的能力,作为凋亡执行蛋白Caspase-3,其激活可活化钙非依赖性磷脂酶A2(calcium-independent phospholipase A2, iPLA2),进而刺激花生四烯酸(arachidonic acid, AA)生成,启动AA代谢途径,后者在环氧合酶(cyclooxygenase, COX)作用下合成前列腺素E2(prostaglandin E2, PGE2)、血栓素A2(thromboxaneA2, TXA2)等因子[8, 9, 10, 11, 12]。这些因子不仅可以促进细胞增殖,黏附和迁移,而且可促进肿瘤间质血管生成,调节肿瘤免疫应答,改变肿瘤微环境,是促使肿瘤复发的重要调质[13, 14, 15]。其中PGE2,可通过激活Wnt/β-catenin通路促进肿瘤干细胞再增殖[16]。Huang等[7]研究发现Caspase在肿瘤中的活性程度与肿瘤患者的恶性预后呈正相关,他们分析了头颈部鳞癌和乳腺癌患者的组织切片中Caspase-3的表达,证明了患者术后复发率与Caspase-3阳性呈正相关。此外,他们还发现在敲除Caspase-3的人乳腺癌细胞系MCF-7荷瘤小鼠模型中,放疗后肿瘤的复发和增殖率显著低于对照组。以上表明Caspase-3是“凤凰涅槃”信号通路强有力的启动因素。此外,Wnt/β-catenin信号通路的激活还可以促进肿瘤的转移和耐药[17, 18],这也暗示Caspase-3介导的“凤凰涅槃”通路不仅导致肿瘤的复发,还能帮助肿瘤抵抗外界的环境,获得更恶性的表型。Chekeni等[19]研究也表明在肿瘤细胞凋亡过程中,Casepase-3的激活可以活化其底物缝隙连接蛋白家族的新成员之一Pannexin 1(Panx 1),从而刺激细胞大量分泌ATP或GTP,招募巨噬细胞清除凋亡细胞的同时分泌多种细胞因子,刺激肿瘤细胞的增殖和存活。
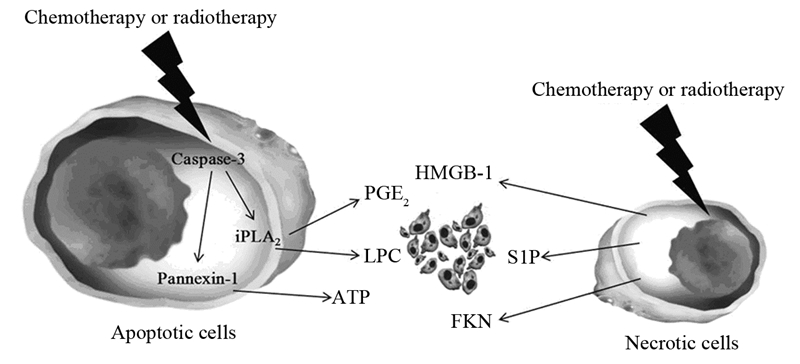
3 活化“凤凰涅槃”通路的其他因素除了Caspase-3-iPLA2-AA-PGE2或Caspase-3-Pannexin 1-ATP/GTP“凤凰涅槃”通路外,濒死的肿瘤细胞还可分泌一些非Caspase介导的细胞因子促进肿瘤复发。Gude等[20]证实肿瘤细胞在凋亡时大量合成一种名为1-磷酸神经鞘氨醇(sphingosine 1-phosphate, S1P)的脂类,可以通过外排小体分泌到肿瘤微环境中,释放信号诱导免疫细胞进行定向清除。但是在这一过程中,S1P本身通过PI3K-Akt信号通路抑制临近肿瘤细胞的凋亡,促进增殖,最终导致肿瘤复发。此外,凋亡细胞亦可分泌一种趋化因子Fractalkine(FKN),通过激活G蛋白偶联受体CX3CR1(CX3C chemokine receptor 1),活化Akt信号通路,促进血管平滑肌细胞的生长,抑制其凋亡,帮助肿瘤细胞复发[21, 22]。另外,坏死细胞释放大量的ATP[23]、溶血磷脂酰胆碱(LPC)[24] 等介质招募肿瘤相关巨噬细胞(tumour-associated macrophages, TAMs),TAMs通过分泌多种促肿瘤生长因子,上调与浸润、转移和血管生成相关的细胞因子和酶,并下调抗血管生成因子的表达量,促进肿瘤的复发[25]。研究表明,由物理或化学损伤引起的肿瘤及基质细胞坏死,使得高迁移率族蛋白-1(HMGB-1)与染色体的结合较疏松,可在坏死细胞中通过破裂的细胞膜被动释放至胞外,进而通过与HMGB-1受体RAGE结合,促进临近黑色素瘤细胞的生长或前列腺癌细胞再增殖[26, 27, 28, 29],这些均为“凤凰涅槃”通路可能的组成部分,见图 1。
|
| 图 1 细胞凋亡或坏死活化“凤凰涅槃”通路 Figure 1 Apoptotic or necrotic cells activate ‘Phoenix Rising’ pathway |
“凤凰涅槃”通路是放、化疗后肿瘤复发的关键环节,而这一新观点提示目前以诱导肿瘤细胞凋亡为主要目的治疗方案或策略面临着巨大隐患。所以,如何平衡化疗药物引起的细胞凋亡和细胞再增殖的关系成为肿瘤治疗亟待解决的问题,阻断 “凤凰涅槃”信号通路是抑制肿瘤复发的新策略。目前的措施主要包括抑制上游Caspase-3的活性,阻断中游iPLA2或者COX-2的表达或者抑制下游以Wnt/β-catenin为代表的肿瘤增殖信号通路。已经证实Caspase-3特异性抑制剂Z-DEVD-FMK等与化疗或者放疗联合可以在治疗肿瘤的同时抑制其复发[30, 31],但注意单独使用Caspase-3特异性抑制剂可在阻断“凤凰涅槃”信号通路的同时,降低诱导肿瘤细胞凋亡的效率。另外,AA代谢途径作为“凤凰涅槃”信号通路的中游,在肿瘤复发中扮演着关键的作用, COX-2抑制剂通过阻断COX活性,抑制PGEs合成[32],抑制了由Caspase-3-iPLA2-AA-PGE2通路激活旁分泌引起的肿瘤复发和转移,为非甾体抗炎药与细胞毒抗肿瘤药物联合应用提供了理论基础。再者,研究表明β-catenin的特异性抑制剂AV-65可以有效抑制Wnt/β-catenin通路信号转导,抑制多发性骨髓瘤细胞的增殖[33]。因此,将β-catenin的特异性抑制剂和化疗或者放疗联合治疗肿瘤将可能成为干预肿瘤细胞死亡引起的复发的又一新手段。
5 总结与展望传统观点认为凋亡仅仅是静态的细胞死亡,不会引起免疫应答,但众多证据表明凋亡细胞可以持续直接或者间接释放一些细胞因子,刺激临近细胞的增殖和分化,作为一个补偿性的生长途径促进受损组织的修复和新生。这种“凤凰涅槃” 现象的发现提示凋亡或死亡细胞在肿瘤复发和转移中的重要作用。因此,阻断 “凤凰涅槃”信号通路则是抑制肿瘤复发和转移的新策略,“凤凰涅槃”信号通路阻断剂和诱导肿瘤凋亡的放、化疗联合应用可以提高肿瘤的治疗效果,减少肿瘤的复发。
| [1] | Hanahan D, Coussens LM. Accessories to the crime: functions of cells recruited to the tumor microenvironment[J]. Cancer Cell, 2012, 21(3): 309-22. |
| [2] | Swartz MA, Iida N, Roberts EW, et al. Tumor microenvironment complexity: emerging roles in cancer therapy[J]. Cancer Res, 2012, 72(10): 2473-80. |
| [3] | Aggarwal BB, Vijayalekshmi RV, Sung B. Targeting inflammatory pathways for prevention and therapy of cancer: short-term friend, long-term foe[J]. Clin Cancer Res, 2009, 15(2): 425-30. |
| [4] | Vakkila J, Lotze MT. Inflammation and necrosis promote tumour growth[J]. Nat Rev Immunol, 2004, 4(8): 641-8. |
| [5] | Ammirante M, Luo JL, Grivennikov S, et al. B-cell-derived lymphotoxin promotes castration-resistant prostate cancer[J]. Nature, 2010, 464(7286): 302-5. |
| [6] | Andreu P, Johansson M, Affara NI, et al. FcRgamma activation regulates inflammation-associated squamous carcinogenesis[J]. Cancer Cell, 2010, 17(2): 121-34. |
| [7] | Huang Q, Li F, Liu X, et al. Caspase 3-mediated stimulation of tumor cell repopulation during cancer radiotherapy[J]. Nat Med, 2011, 17(7): 860-6. |
| [8] | Galluzzi L, Kepp O, Kroemer G. Caspase-3 and prostaglandins signal for tumor regrowth in cancer therapy[J]. Oncogene, 2012, 31(23): 2805-8. |
| [9] | Li F, Huang Q, Chen J, et al. Apoptotic cells activate the" phoenix rising" pathway to promote wound healing and tissue regeneration[J]. Sci Signal, 2010, 3(110): ra13. |
| [10] | Zhao X, Wang D, Zhao Z, et al. Caspase-3-dependent activation of calcium-independent phospholipase A2 enhances cell migration in non-apoptotic ovarian cancer cells[J]. J Biol Chem, 2006, 281(39): 29357-68. |
| [11] | Zhang M, Xu ZG, Shi Z, et al. Inhibitory effect of celecoxib in lung carcinoma by regulation of cyclooxygenase-2/cytosolic phospholipase A2 and peroxisome proliferator-activated receptor gamma[J]. Mol Cell Biochem, 2011, 355(1): 233-40. |
| [12] | Xu Z, Zhang M, Lv X, et al. The inhibitory effect of celecoxib on mouse hepatoma H22 cell line on the arachidonic acid metabolic pathway[J]. Biochem Cell Biol, 2010, 88(4): 603-9. |
| [13] | Schneider C, Pozzi A. Cyclooxygenases and lipoxygenases in cancer[J]. Cancer Metastasis Rev, 2011, 30(3-4): 277-94. |
| [14] | Bai XM, Zhang W, Liu NB, et al. Focal adhesion kinase: Important to prostaglandin E2-mediated adhesion, migration and invasion in hepatocellular carcinoma cells[J]. Oncol Rep, 2009, 21(1): 129-36. |
| [15] | He YF, Jin J, Wei W, et al. Overexpression of cyclooxygenase-2 in noncancerous liver tissue increases the postoperative recurrence of hepatocellular carcinoma in patients with hepatitis B virus-related cirrhosis[J]. Can J Gastroenterol, 2010, 24(7): 435-40 |
| [16] | Goessling W, North TE, Loewer S, et al. Genetic interaction of PGE2 and Wnt signaling regulates developmental specification of stem cells and regeneration[J]. Cell, 2009, 136(6): 1136-47. |
| [17] | Fodde R, Brabletz T. Wnt/beta-catenin signaling in cancer stemness and malignant behavior[J]. Curr Opin Cell Biol, 2007, 19(2): 150-8. |
| [18] | Christie M, Jorissen RN, Mouradov D, et al. Different APC genotypes in proximal and distal sporadic colorectal cancers suggest distinct WNT/beta-catenin signalling thresholds for tumourigenesis[J]. Oncogene, 2013, 32(39): 4675-82. |
| [19] | Chekeni FB, Elliott MR, Sandilos JK, et al. Pannexin 1 channels mediate ‘find-me’ signal release and membrane permeability during apoptosis[J]. Nature, 2010, 467(7317): 863-7. |
| [20] | Gude DR, Alvarez SE, Paugh SW, et al. Apoptosis induces expression of sphingosine kinase 1 to release sphingosine-1-phosphate as a “come-and-get-me” signal[J]. FASEB J, 2008, 22(8): 2629-38. |
| [21] | Truman LA, Ford CA, Pasikowska M, et al. CX3CL1/fractalkine is released from apoptotic lymphocytes to stimulate macrophage chemotaxis[J]. Blood, 2008, 112(13): 5026-36. |
| [22] | Gregory CD. Inflammation and cancer revisited: an hypothesis on the oncogenic potential of the apoptotic tumor cell[J]. Autoimmunity, 2013, 46(5): 312-6. |
| [23] | Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer[J]. Cell, 2010, 140(6): 883-99. |
| [24] | Lauber K, Bohn E, Krober SM, et al. Apoptotic cells induce migration of phagocytes via caspase-3-mediated release of a lipid attraction signal[J]. Cell, 2003, 113(6): 717-30 |
| [25] | Daurkin I, Eruslanov E, Stoffs T, et al. Tumor-associated macrophages mediate immunosuppression in the renal cancer microenvironment by activating the 15-lipoxygenase-2 pathway[J]. Cancer Res, 2011, 71(20): 6400-9. |
| [26] | Bustin M. Regulation of DNA-dependent activities by the functional motifs of the high-mobility-group chromosomal proteins[J]. Mol Cell Biol, 1999, 19(8): 5237-46. |
| [27] | Bianchi ME, Beltrame M. Upwardly mobile proteins. Workshop: the role of HMG proteins in chromatin structure, gene expression and neoplasia[J]. EMBO Rep, 2000, 1(2): 109-14. |
| [28] | Yanai H, Ban T, Wang Z, et al. HMGB proteins function as universal sentinels for nucleic-acid-mediated innate immune responses[J]. Nature, 2009, 462(7269): 99-103. |
| [29] | Venereau E, Schiraldi M, Uguccioni M, et al. HMGB1 and leukocyte migration during trauma and sterile inflammation[J]. Mol Immunol, 2013, 55(1): 76-82. |
| [30] | Mao P, Smith L, Xie W, et al. Dying endothelial cells stimulate proliferation of malignant glioma cells via a caspase 3-mediated pathway[J]. Oncol Lett, 2013, 5(5): 1615-20. |
| [31] | Cheng J, Tian L, Ma J, et al. Dying tumor cells stimulate proliferation of living tumor cells via caspase-dependent protein kinase Cδ activation in pancreatic ductal adenocarcinoma[J]. Mol Oncol, 2014, 9(1): 105-14. |
| [32] | Bowers LW, Maximo IX, Brenner AJ, et al. NSAID use reduces breast cancer recurrence in overweight and obese women: role of prostaglandin-aromatase interactions[J]. Cancer Res, 2014, 74(16): 4446-57. |
| [33] | Yao H, Ashihara E, Strovel JW, et al. AV-65, a novel Wnt/beta-catenin signal inhibitor, successfully suppresses progression of multiple myeloma in a mouse model[J]. Blood Cancer J, 2011, 1(11): e43. |
 2015, Vol. 42
2015, Vol. 42


